
When Allen D. Beck stops to think about what it takes to helm the Emory Eye Center and Department of Ophthalmology, he has a lot to draw upon. He readily admits that much of his own leadership is steeped in the wisdom of those who came before him. He is quick to call out one of them, Dr. Paul Sternberg Jr. who will be delivering the Henry Edelhauser lecture to graduating residents and fellows on June 8.
“Paul had a way of impressing upon residents and fellows the importance of anticipating details and preparing for them,” Beck recalls. “It wasn’t just that the work is tough and it demands precision. It’s that preparation on all levels means better care for the patients. As a mentor, he always stressed the importance of the patient above all things.”
This simple dictum must have remained in the forefront of Sternberg’s thoughts when he left Emory to establish the Vanderbilt Eye Institute more than 20 years ago. His success – as a chair, chief medical officer, and chief patient experience officer– put his career in a league of its own. He was even recruited to assume a new leadership role – medical director of development – after he officially retired in 2023.
What his resume cannot explain is how Paul Sternberg, Jr. did it all. So we asked him to fill in some of the space between ambition and action. What we found was man committed to harvesting valuable lessons from both triumphs and failures. Fortunately, he’s had more of the former.

What’s the most important thing our graduating residents and fellows can do when they land in their next job?
New jobs mean a new start, which is a great opportunity for self-reflection and self-improvement. It’s actually easier to do both in a new environment. So if you’re a resident or a fellow, now’s the time to pause, look at yourself, and ask “What can I do better than I did at the last place?” It doesn’t have to be a wholesale change but take advantage of the opportunity. Above all else, don’t be arrogant enough to think that because they gave you the job, you have nothing to Improve.
My own experience with this came very early. When I was 15, I moved from my public high school to a private boarding school. One of the reasons I made the change was that I was really struggling to find a social group. I was very shy, and I was uncomfortable in my own skin. When I went to the new school, I said to myself “Nobody knows you as this kind of nerdy, shy, short kid. You can be whoever you want to be.” So, the first day in the dorm, I knocked on everyone’s door and introduced myself. I said, “I’m Paul, and I’m from Chicago, and I’m one of the new students and I’m really excited to be here.”
It was the hardest thing I’ve ever done in my life. I intentionally converted myself from an introvert to an extrovert. And it has helped me grow into virtually every role I have taken on during the course of my career.
You’ve mentored a lot of clinicians in your time. What makes a good mentor?
In my career, I’ve learned about mentorship by learning about leadership. The key to both, I believe, is listening.
At Vanderbilt, I started out as chair, but was eventually recruited for chief medical officer and chief patient experience officer – two roles that I in no way sought and for which I didn’t even apply. I remember telling the Dean/CEO that, of course, I would have to step down from my job as chair to become CMO, but he said that wasn’t the plan. He said he wanted me to be a player-coach – someone who could coach the other chairs.
None of those chairs reported to me, so how was I going to get them to do stuff for me or at least support the institutional initiatives I was asked to lead?
That’s when I learned the concept of leadership by influence – rather than leadership by authority. Medicine is normally very hierarchical, with defined roles and lines of authority. Instead of issuing orders, my new roles required me to first build a solid base of trust that would convince my colleagues that a new initiative or task was the right thing to do.
It obviously helped that the that the CEO and dean at Vanderbilt had already displayed his confidence in me, but I had to take it a step further. I had to build trust. I met regularly with these chairs and did a lot of listening. When a problem was brought up, my natural tendency was to try to fix it, but I learned to hold back. I listened for the answers that were already there. Instead of trying to identify what should be done, I would say “Well, what do you think you should do? What does your instinct tell you is the best way to solve this. Let's talk through it.”
What I found was, most of them knew exactly what they needed to do. And it was rare where I had to act or restructure their thoughts about a process. And, even when I would do that, instead of saying, “Well, I think you're wrong, try it this way.” It would be “Well, what if you thought about it this way? How would that change how you would approach your solution?”

And what makes a good protege?
We learn and we grow from our mistakes. One of the challenges I faced in mentoring folks over the years is in determining whether they have self-awareness -- a recognition of their shortcomings -- and a willingness to address them. Fortunately, most people with whom you work in a mentoring relationship have this desire or ability. They want to improve, so they are willing to challenge themselves. But even then, it is a matter of degree. In the end, the more confident a person is in challenging himself the more she or he will grow.

What was the hardest part of the transition from being a clinician at Emory to an administrator at Vanderbilt?
(Laughs) At Emory, where I developed some wonderful relationships, I know I had a reputation for being fire-y, for losing my temper. On the one hand, some of that came from my focus on the patient and the importance of being prepared, of not letting things slip through the cracks because the patient would suffer. But I knew that wouldn’t work if I wanted to be successful in my career. So when I came to Vanderbilt as the new chair, I made the conscious decision to control my temper, to press the pause button when things weren’t going my way.

How did that work?
I’ve had some feedback over time that has encouraged me.
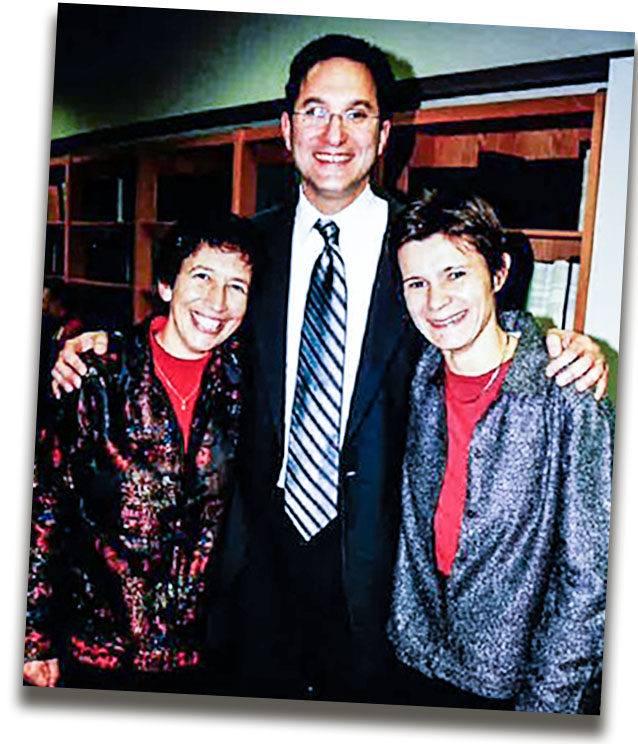
A few years ago, when we built the Eye Institute [at Vanderbilt], a number of my former trainees came to celebrate the opening. And of course, when we went out for drinks, they wanted to share war stories. When some of them alluded to times in the past when I had lost my temper – and they did so as friends -- my current faculty colleagues were confused. They kept saying ‘What are you talking about?’ because they’d never seen me behave that way.
Later, during an annual evaluation, the dean asked all of the chairs to pick a few things we view as challenges. I put down ‘losing my temper.’ When he read it, he said “What are you talking about? I see you in meetings as the Chief Medical Officer when the other chairs are going out of their way to provoke you. And you are always the calmest person in the room. You never let them get under your skin.”
They did provoke me, all the time. But I did not see the utility of letting them know that.
And much more recently, I was asked to run the COVID Command Center for the Medical Center, a job that had all the potential in the world to provoke tempers in me and everyone around me. I was the one who would have to sit down with the chief of staff who was totally freaking out and tell him that we’d get things under control. There was no room in that situation for the surgeon I was 20 years earlier– the guy who would throw a fit because another doctor did not have the laser ready. During COVID, we often found ourselves flying without radar, but my job was to keep a steady, calm message coming out to the medical community while we looked for answers. We couldn’t afford to let anger or fear turn to panic.

You have achieved professional goals that elude many very ambitious doctors. What keeps you humble in the face of such success?
Humility is a deft and exacting teacher.
When I was a resident, at Johns Hopkins I and a good friend were both competing to be named chief resident. At the time, being named chief resident was a real stepping-stone for your career, and it was very competitive. When it was announced that I had been named, my friend told me that he was disappointed that he hadn’t at least been named co-chief, but that I was better organized and had better administrative skills for the job. He wished me well.
I felt terrible. Really terrible.
And the reason is this: when he said that, I had to ask myself if I would been as gracious if he’d been chosen? The answer, I knew right away, was no. I’d have been angry and disappointed. That was the truth, at that time, as a young doctor. And it was something I worked to change throughout my career.
Your Emory legacy lives on through the fond memories of your former colleagues as well as the Paul Sternberg, Jr. Endowed Lectureship. Why was it important for you to express your philanthropy to Emory through an endowed lectureship?
The lectureship is very important to me, personally and professionally.
It started when I was appointed to head the Retina Division by Dr. Aaberg. I was just three or four years into my time at Emory, and I wanted to make our Retina Division world-class. So, every time I was given an honorarium for speaking or did any consulting work, I would donate the money to the Emory Lecture Fund, which, I hoped would allow us to bring in top retina experts to speak. The SEVR [Southeastern Vitreoretinal Seminar] was another thing I started for the same reason: I wanted retina experts to recognize Emory, to come here to see what we were doing. When I was promoted to full professor, Dr. Aaberg asked me to come to his office. He said he wanted to introduce me to a very special donor who had been impressed by my work and wanted to endow the lectureship for good.
That person was my wife, Gloria.
interview by Kathleen E. Moore

