About the Program
The Neurologic Physical Therapy Residency Program at Emory University was developed to provide clinicians interested in pursuing specialty practice in neurologic physical therapy a concentrated, structured experience including clinical, didactic, service, research and teaching components. The program is designed to prepare residents for the national board examination (American Board of Physical Therapy Specialties) required to become a certified Neurologic Clinical Specialists.
Requirements for Success
- Complete a minimum of 1500 clinical hours
- Complete 150 hours of 1:1 mentoring
- Complete 300 hours combined of didactic, research and teaching
- Achieve a passing score on all residency assessments
Curriculum
At-A-Glance
- Practice in a variety of clinical settings spanning the continuum of care in neurologic rehabilitation.
- Teach entry-level students in Emory University’s DPT program.
- Complete didactic coursework in collaboration with the Neurologic Physical Therapy Professional Education Consortium.
- Practice in local service-learning programs.
- Participate in a neurologically focused research project.
Program Goals
- Emory Neurologic Physical Therapy Residency Program will provide the necessary content and clinical experiences to prepare the resident for successful completion of the ABPTS specialist certification examination.
- Emory Neurologic Physical Therapy Residency Program will build the resident’s skills in teaching and mentoring.
- The Emory Neurologic Physical Therapy Residency Program will engage residents in activities supporting research and use of evidence to guide clinical decision making.
- The Emory Neurologic Physical Therapy Residency Program demonstrates commitment to the health and wellbeing of each resident.
- The program will provide a curriculum that prepares residents for specialized clinical practice in neurologic physical therapy and prepares residents for successful completion of the Board examination in neurologic physical therapy.
- The program will operate in a manner which is sustainable and financially solvent over time.
Didactic Learning
The didactic portion of our program includes onsite, webinar, and journal club sessions. By collaborating with the Neurologic Physical Therapy Professional Education Consortium, resident participate in high quality didactic content and network with residents and residency faculty from programs throughout the country.
In addition to completing a clinical rotation in vestibular rehabilitation, our residents may opt to complete an intense, evidence-based, six-day course: Vestibular Rehabilitation: A Competency-Based Course.
Clinical Care
Emory Healthcare, our primary clinical partner, is an integrated academic health system committed to upholding our core principles of excellence, caring and integrity providing outstanding quality care in some of the highest ranked healthcare facilities in the world. Residents will complete a series of rotations within Emory Healthcare clinics and hospitals providing care to patients with neurologic diagnoses across the continuum including: acute care/neuro ICU, inpatient rehabilitation, outpatient rehabilitation, vestibular rehabilitation and movement disorders.
Residents will experience specialty clinical care in a variety of sites across the healthcare system. The clinical sites are selected specifically for their clinical excellence, collaborative and experienced staff, outstanding mentorship and the ability to provide residents exposure to diagnoses included in the APTA Description of Specialty Practice in Neurology. Residents learn from expert mentors in each sub-specialty area of clinical practice included in the program.
Our current partners include:
The Emory Clinic
Research
Residents are encouraged to pursue research experiences based on their individual interests. In addition to research within the Division of Physical Therapy (Emory DPT research), residents may also benefit from our discovery collaborations with:
Teaching
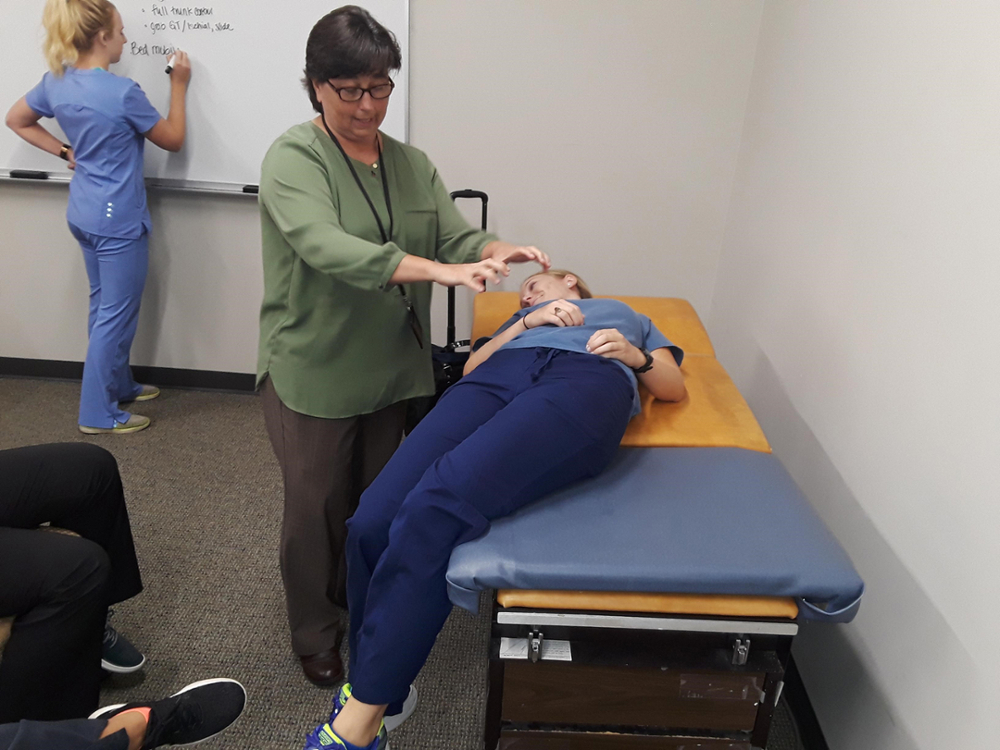
Residents teach in the Emory DPT program Fall semester in the Adult Neurorehabilitation Course. This is a 12-credit clinical complex required for second year DPT students. Residents assist in labs, lectures, exam item writing and grading of practical exams, written exams and assignments. Teaching mentorship is provided to the residents via faculty and student feedback.
Service Learning
Residents participate in a local pro bono clinic which offers quarterly rehabilitation to adults with stroke and brain injury who do not have funding for traditional clinic services.
A Day in the Life of a PT Resident
- 30-40 hours of clinical practice per week
- 3 hours of 1:1 clinical mentoring per week
- Research four hours per week (January-August)
- 8 hours of teaching per week in Emory’s DPT program (August-November)
- Didactic coursework (onsite sessions, webinars and journal club sessions)
Admissions
All applications must be submitted through RF-PTCAS. Application cycle begins annually in October.
Requirements include:
- Graduate of a CAPTE accredited doctor of physical therapy program
- Georgia Physical Therapy license and in good standing with the State Board
- Current curriculum vitae or resume
- Current CPR certification
- APTA membership strongly encouraged
Please visit the American Board of Physical Therapy Education Residency and Fellowship website for additional information regarding application deadline and content submission.
Resident Professional Contributions
Keenan Whitesides
Publications:
- “The Choice” published in The Intima
- “Enough Said” published in Journal of Humanities in Rehabilitation
Poster:
- Evaluating Relationships between Lesion Characteristics and Upper Extremity Impairment in Chronic
- Expanding stroke telerehabilitation services to rural veterans: a qualitative study on patient experiences using the robotic stroke therapy delivery and monitoring system program
Posters:
- Fostering Critical Thinking Skills by Bridging Science with the Art of Patient Care
- Daily Acute Intermittent Hypoxia Enhances Self-Selected Walking Speed in Persons with Chronic Incomplete Spinal Cord Injury
- Suggested Guidelines for Backwards Walking Speed: Scoring The Functional Gait Assessment
Publication:
- Mind Mapping: Using Visual Thinking to Improve Patient Care and Quality of Life
- Assessment of gait abnormalities in individuals with Parkinson’s Disease and suspected Cholinergic deficits
Publication:
- Effects of real-time gait biofeedback on paretic propulsion and gait biomechanics in individuals post-stroke.
- Objective Evaluation of Upper Extremity Proprioception Sense in Individuals with Spinal Cord Injury
Sydney Bricker
- The Relationship Between Cognitive Domains and Gait Performance in People with Mild Cognitive Impairment and Alzheimer’s Disease
Brittney Hooker
Poster:
- Effects of Fast FES Training on Motor Learning During Post-Stroke Gait Rehabilitation
Poster:
- Effects of Fast FES Training on Motor Learning During Post-Stroke Gait Rehabilitation
Poster:
- Effects of Fast FES Training on Motor Learning During Post-Stroke Gait Rehabilitation
- HIV, opioids, and chronic pain
Rosie Kelly
- Neuroplasticity and Biomechanical Correlates Underlying Post Stroke Gait Rehabilitation
Siobhan Pfaff
- Is a simple measure of upper extremity strength indicative of post-acute discharge destination after stroke?
Vincent Santucci
- Effects of real-time gait biofeedback (AGRF vs TLA) regarding limb position versus push-off force generation on post-stroke gait biomechanics
Grace Couture
- Patient-Centered Pressure Ulcer Outcome Preferences: A Mixed-Methods Study
Kimberly Bader
- Relationship between gait parameters and progression of disease from Mild Cognitive Impairment to Alzheimer’s Disease
Payton Sims
Publication:
- Is Faster Always Better? A Subgroup Analysis of the Effects of Walking Speed on Post-Stroke Gait Biomechanics
Shantha Nithiananda
- Predictive Value of Mini-BESTest Subdomains for Future Falls in Patients with Parkinson’s Disease
Christine Cook
Poster:
- Feasibility of PREP2 Algorithm in US Healthcare System
Shannon Fillmore
- PD Circumstances of self-reported falls in Parkinson’s disease
- Exploring the relationship Between Non-Motor Symptoms and Balance in Individuals with Parkinson’s Disease
- Protocol for tele-health model of physical therapy to prevent opioid use disorder (OUD) and mitigate chronic pain in people living with HIV (PWH)
- Spatial Neglect and Prism Adaptation Treatment
Olivia Schipani
- Gait Variability a predictor of fall risk in Early Onset Alzheimer’s Disease
Kayla Brennan
Poster:
- Evaluation of a Carepartner-Integrated Telehealth Gait Rehabilitation Program for Persons with Stroke
Sarah Roberts
Poster:
- Greater Non-Paretic Limb Loading Is Associated with Lower Clinical and Reactive Balance Function Post-Stroke
Macie Sims
- Evaluating Participant Recruitment for Subacute Stroke Rehabilitation Research






