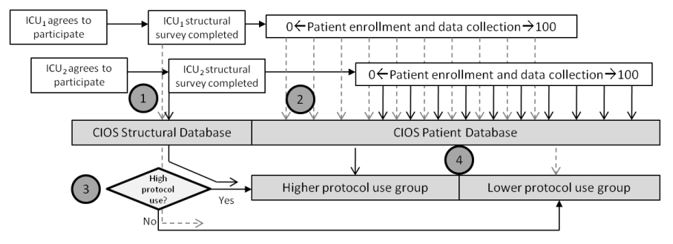
Based on the principles of Donabedian, the quality and value of ICU health care are affected by the structure and processes inherent locally to an ICU and more generally to the hospital and the organization in which the ICU operates. For example, a “closed” ICU organizational structure is generally observed to produce better outcomes at a lower cost than an “open” ICU, and introduction of a “daily goals of care” process has been shown to decrease surgical ICU length of stay. Importantly, however, there are conflicting reports, such as improvements in outcomes for patients cared for in an ICU with newly developed protocols even if the protocols were not applied to the patients of interest. In order to better understand the heterogeneity in organizational structure and processes across intensive care units and how these factors contribute to relevant clinical outcomes, Jonathan Sevransky, MD; Dr. William Checkley, MD; and Greg Martin, MD launched CIOS, the Critical Illness Outcomes Study (NCT01109719) under the aegis of the US Critical Illness and Injury Trials Group (USCIITG).
The CIOS study was designed as a multi-centered ecological study of patients cared for in critical care units across many types. Overall, there were approximately 6,500 patients enrolled from 69 ICU’s geographically spread across the United States. The CIOS study has generated multiple manuscripts, such as:
-
Describing the complexity of executing a multi-centered study where data is collected on both an organizational level (structure and processes) and at a patient level (data collected on individual patients cared for in study ICU’s)
-
Discussion and comparison of the both the consistent and variable processes in conducting multi-site studies in critical care, particularly as it relates to interpretation of ethical regulations by institutional review boards
-
Identifying the associations between better clinical outcomes and structure and process variables such as the nurse:patient ratio and incorporation a daily plan of care into ICU rounds
-
The relationship between protocols and outcomes at the patient level in medical, surgical and mixed ICU's

