All members of the Emory Program in Critical Care (EPICC) group have studied the epidemiology of various critical illnesses, most often examining these conditions from a national perspective using administrative data. Collaborations with investigators at the Centers for Disease Control and Prevention (CDC) facilitated our early work in this area, and these have continued to grow. In addition to the work described below, we have also generated important data related to venous thromboembolism, cardiac arrest, and pulmonary artery catheterization.
Incidence, Outcome, and Health Disparities in Sepsis

We began by examining the longitudinal epidemiology of sepsis, with particular attention to changes in incidence and mortality. At the time, Dr. Greg Martin’s work produced the first national estimates of sepsis for the United States, showing it to be at least the tenth leading cause of death in our country and having been rising to that status over the preceding 25 years.
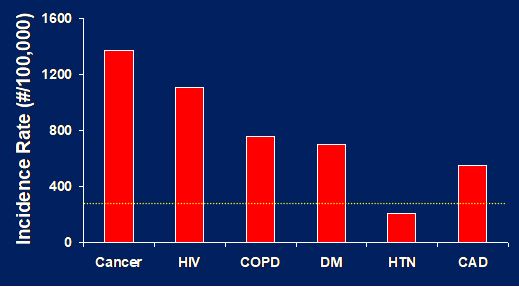
At that time, we also reported disparities in the incidence of sepsis based upon race and gender, with non-Caucasians having nearly a doubling of their risk for sepsis and males having an approximate 30 percent increase. Investigators in our group have followed these original reports to further describe the effect of age on sepsis, with incidence increasing exponentially around the age of 60 years. Together, we also examined the role of co-morbidities in sepsis and associated these chronic co-morbid medical conditions with the identified healthcare disparities.
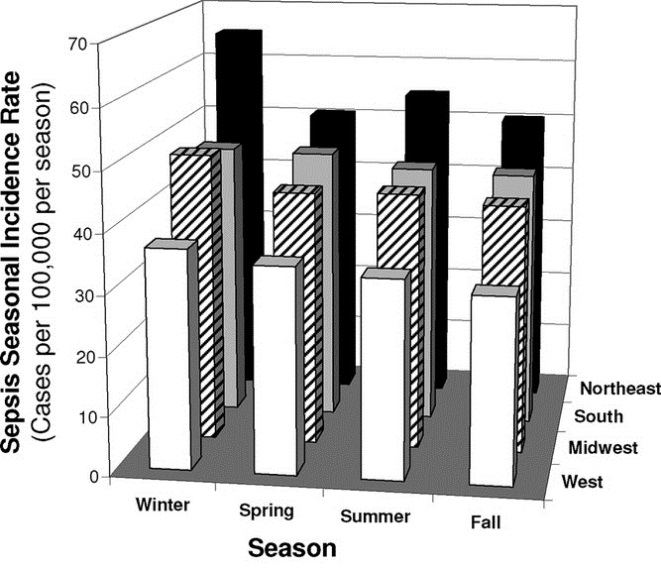
In addition, we also described both seasonal and regional differences in the incidence and outcome of sepsis, and specific association of seasonal changes in sepsis to viral respiratory infections.
Epidemiological Assessments of ARDS
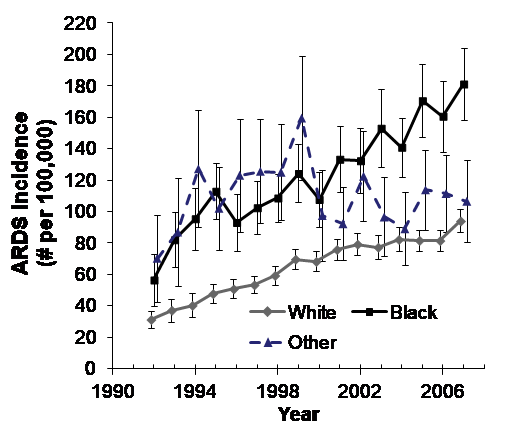
Using nationally representative administrative data, researchers in our group were the first to report national estimates of ARDS mortality including differences in mortality according to race. We have followed those original observations with additional assessments of both secular changes in ARDS incidence and changes in mortality in collaboration with colleagues from the CDC, investigators from the NIH-funded ARDS Network, and in collaboration with colleagues from the University of Michigan.
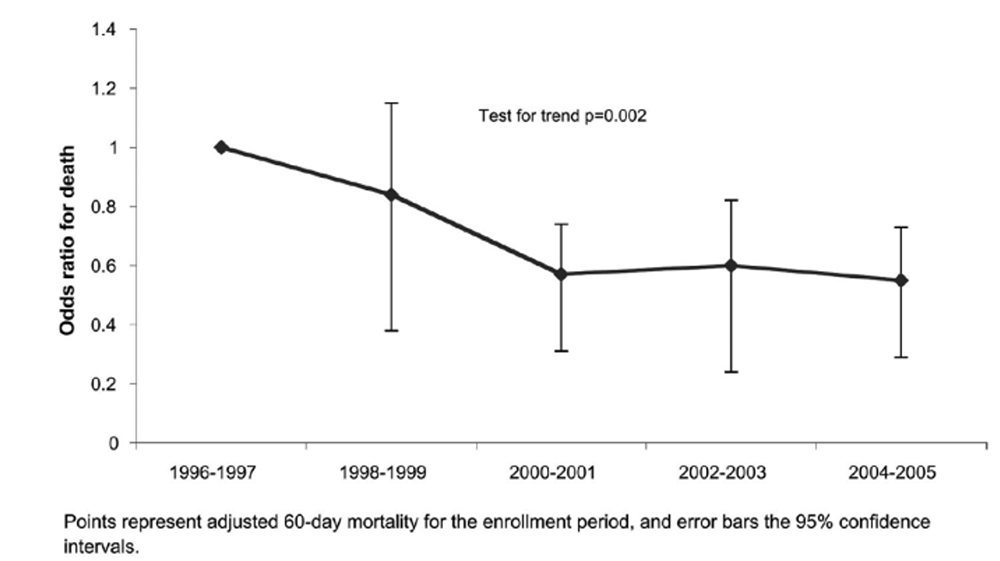
We continue to study health disparities with ARDS, as both a contributor to differences in disease incidence as well as in outcomes with ARDS. Our interests are to better understand longitudinal changes in disease incidence and outcome, to describe and understand healthcare disparities in critical care, and to better characterize the healthcare resources applied to various critical illnesses through this work.
Examination of Health Disparities in Critical Illnesses and Injuries
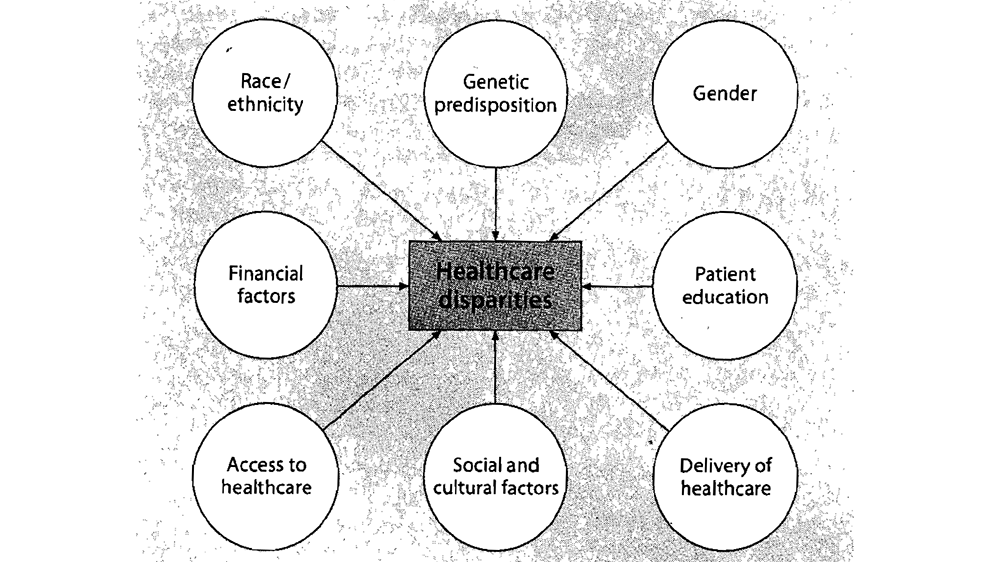
Despite the tremendous technological advancements in the recent history of medicine, disparities in healthcare continue to exist. The preponderance of peer-reviewed literature on healthcare disparities focuses on conditions in the U.S. and much attention has been focused here because of the National Academy of Sciences Institute of Medicine publication entitled, “Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare.”
Disparities in ICU patients are often less recognized, as efforts to identify and eliminate disparities frequently focus on common clinical conditions. In the U.S., non-White patients are generally reported to receive less intensive hospital care compared to others, and it has been observed that after controlling for hospital and insurance plans, non-White patients with the same diagnosis are less often admitted to intensive care units. Despite these differences, it remains uncertain if non-White patients, once admitted to the ICU, receive different care, and if so, the factors that account for these differences. We have demonstrated that Black patients suffer from an age-dependent 2-3 fold increase in the risk of sepsis and sepsis-related mortality with the greatest disparity among 35-44 year-olds, and that Black patients with sepsis have greater frequency of concomitant diabetes mellitus, chronic kidney disease, human immunodeficiency virus (HIV), and alcohol abuse.
As we delve into the factors that may contribute to disparities in both incidence and outcome, we are also exploring urbanicity, relationship with hospital quality, and socioeconomic risk factors. Greater efforts are required to characterize the magnitude of healthcare disparities in critically-ill patients and to seek the root causes of these disparities. The elimination of healthcare disparities will require different interventions depending on the type of disparities, the underlying cause(s) and the type of healthcare system in which they occur.

