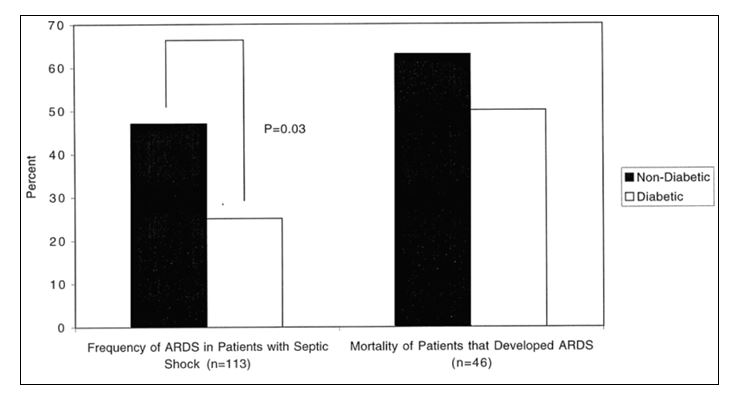
Acute lung injury (ALI) is a common condition occurring in as many as 25% of mechanically ventilated patients and is associated with significant morbidity and mortality. The inflammatory response in ALI is driven by activation of key signaling pathways that involve alveolar macrophage (AM) responses, activation of transcription factors, oxidative stress, and cytokine release. Predisposing factors for sepsis (age, chronic liver disease, HIV, cancer) may not equally contribute to the risk of ALI, as not all critically ill patients develop ALI. Of the disorders commonly associated with the development of ALI, sepsis carries the highest risk at approximately 40%. Annette Esper, DO has investigated specific co-morbid conditions that are disproportionately observed in the sepsis population. Diabetes mellitus (DM) is a common co-morbid condition in critically ill patients, present in 17% of patients with sepsis. A prospective cohort study conducted by our research group was the first to document that diabetic patients who develop sepsis are at lower risk for developing ALI compared to non-diabetics. To broaden our understanding of diabetes and its influence on acute organ dysfunction with sepsis, Esper aggregated multi-year national hospitalization data and reported that sepsis patients with diabetes were consistently less likely to develop respiratory failure than sepsis patients without diabetes. These findings have now been independently reproduced in at least two prospective cohort studies.
To investigate further this association between DM and ALI, Esper designed a prospective cohort study of patients with severe sepsis in order to elucidate clinical factors, such as anti-diabetic medications and glycemic control, as factors influencing the development of ALI in diabetics. A priori, the scientific hypothesis was that specific clinical factors such as prehospitalization glucose control, or exposure to specific anti-diabetic medications such as insulin and thiazolidinediones (TZDs), would impact the development of ALI and would lead to further studies on better defining the mechanisms by which these factors alter ALI risk.
This unexpected finding that people with diabetes mellitus have a decreased incidence of ALI during sepsis is intriguing. Although there are many potential explanations for this apparently paradoxical association, there are compelling reasons to hypothesize that increased activation of the peroxisome proliferator-activated receptor gamma (PPARg) in the AMs of individuals with diabetes could limit acute alveolar injury and promote more rapid resolution of inflammation within the alveolar space. Our preliminary data suggest that PPARg activity, a key regulator of AM activation, is increased in otherwise healthy diabetics. If this is true, then the relative PPARg activation in the AM should correlate with the risk of ALI in diabetics, but also in nondiabetics as well. Most importantly, PPARg activation represents an attractive therapeutic target that could decrease the incidence or severity of acute lung injury in diabetics and nondiabetics with sepsis or other acute stresses. To further investigate the role of PPARg, we are currently conducting a study to determine the association between AM PPARg activity and ALI in patients with severe sepsis, independently of underlying diabetes; and to characterize the effect of PPARg activity on AM phenotype and function in these patients.

