Sepsis is a significant public health problem that affects nearly one million people every year in the United States. It is an acute inflammatory response to an infection, leading to systemic illness and organ dysfunction, which is a primary determinant of survival. However, the development of organ dysfunction is highly variable in sepsis patients and not predicted by clinical or physiological variables. Of the mechanisms that lead to sepsis-related organ dysfunction and death, alterations in vascular function are a primary contributor. Early descriptions of endotoxin induced vascular reactions showed that changes in vascular hemodynamics were influential in accounting for the poor responses of animals to endotoxin. Since then, many experimental studies have reported and discussed the microvascular alterations that occur in sepsis and more recently, alterations in microvasculature have been reported in human subjects with sepsis and have correlated with severity of disease. Damage to the endothelium can result in multi-organ failure, which can lead to increased severity of sepsis, and ultimately increase mortality. Stem cells from the bone marrow may contribute to endothelial repair, migrating from the bone marrow to the peripheral circulation where they contribute to vascular repair. When injected into animal models of ischemia, stem cells are incorporated into sites of neovascularization and have even improved outcomes in critically ill patients.
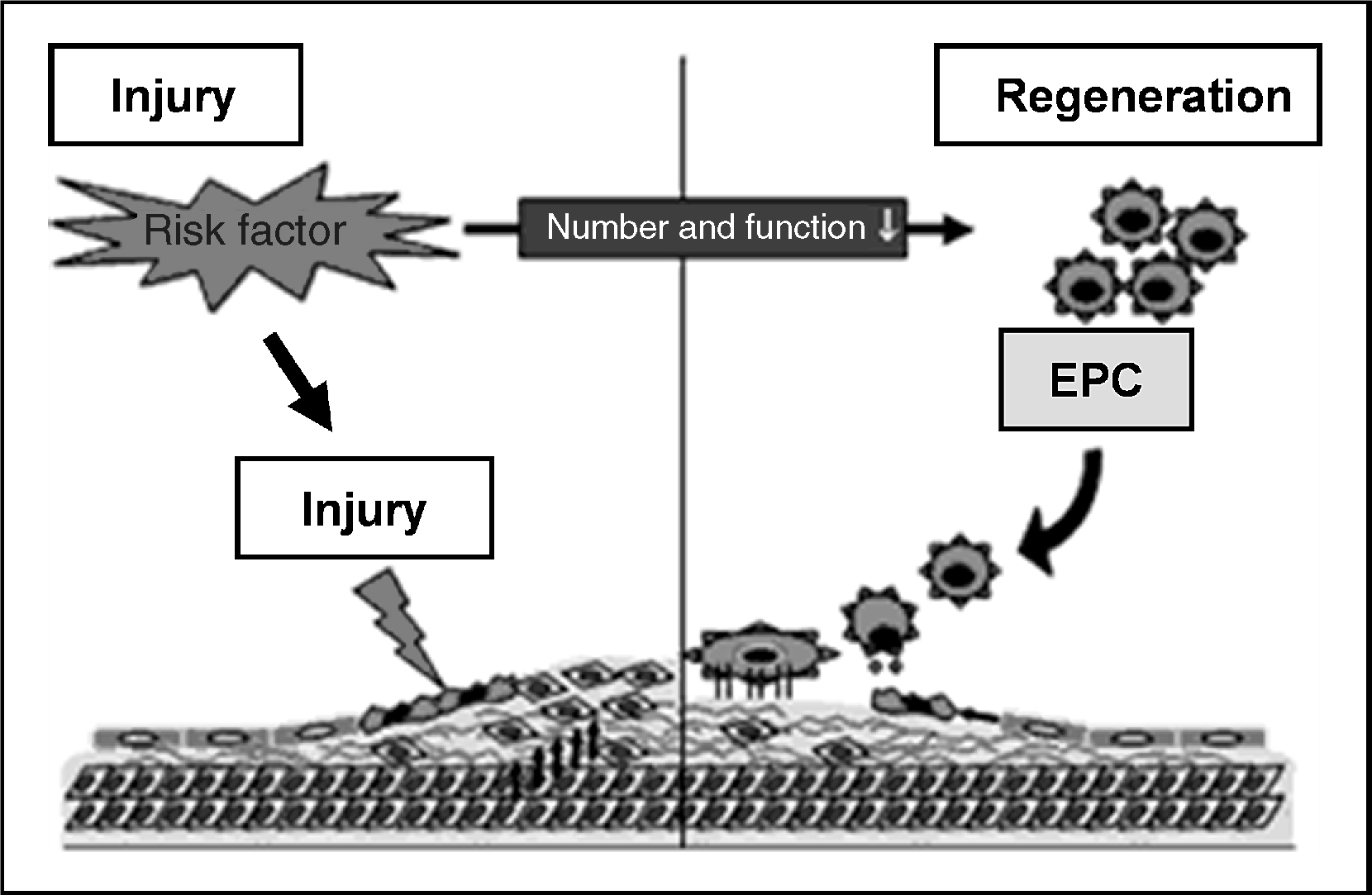
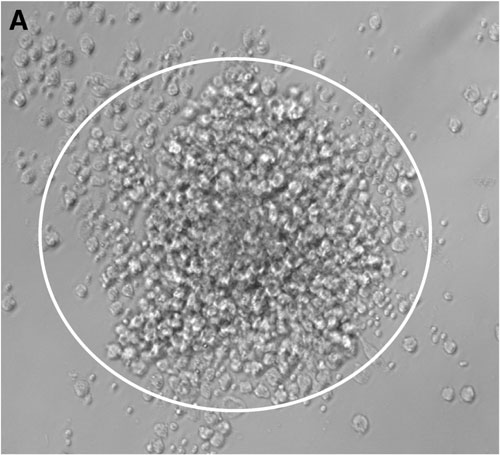
Our group at Emory University includes Sushma Cribbs, MD; Greg Martin, MD; and W. Robert Taylor, MD, among other collaborators throughout the university, as well as external to Emory. We have been interested in bone marrow derived progenitor or stem cells for many years, both in experimental animal models and clinically relevant human studies. We have shown that infusion of bone marrow derived mesenchymal stem cells abrogates lung injury in a murine LPS sepsis model and that circulating endothelial progenitor cells correlate prognostically with organ dysfunction in a cohort of sepsis patients and with survival in a cohort of acute lung injury patients. Understanding the function of stem cells in sepsis and sepsis-related organ dysfunction (such as acute lung injury), and the relationship to various cytokines and growth factors, may provide innovative diagnostic and therapeutic approaches in this devastating disease.

