BEHAVIORAL MENTAL HEALTH TRACK (2 positions)
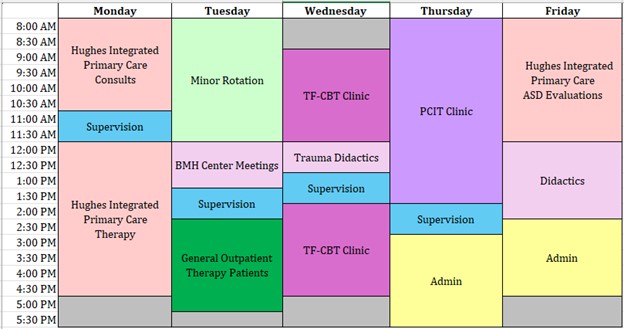
The Behavioral and Mental Health Track at Children’s Healthcare of Atlanta seeks to ensure patients receive access to behavioral and mental health services that will improve their quality of life and ability to thrive. Interns spend time in the Outpatient Clinic at the Zalik BMH Center as well as the Integrated Primary Care Clinic at Hughes Spalding.
The BMH Outpatient Clinic serves a general child clinical and adolescent population referred from internal Children’s specialty medical clinics and aims to increase the continuity of care available to Children’s patients to include behavioral and mental health care. The outpatient clinic serves children with a broad range of presenting concerns including anxiety, mood disorders, persistent post-traumatic stress symptoms, somatic symptoms, developmental disabilities, and behavioral problems. Many patients have comorbid medical conditions and are referred from specialties such as endocrinology, oncology, neurology, transplant, chronic pain, adolescent medicine, and orthopedics. A multi-disciplinary team of psychologists, mental health therapists, social workers, nurse practitioners, and physicians provide both assessment and treatment services for children. Treatment modalities include individual therapy, group therapy, family therapy, and parent training. Evidence based practices such as cognitive behavioral therapy, acceptance and commitment therapy, parent-child interaction therapy, and trauma-focused cognitive behavioral therapy are used. Medication management is provided as needed for patients. Interns will participate in monthly multidisciplinary case consultations and staff meetings. The following is a menu of options of available rotations within the BMH Outpatient Clinic:
- General Outpatient Therapy – Provide intervention to patients from general BMH waitlist, tend to be adolescents with internalizing disorders
- PCIT Clinic - Learn PCIT Intervention and carry a caseload of approximately 4 PCIT cases
- Trauma Clinic - Learn TF-CBT Intervention and carry a caseload of approximately 4 TF-CBT cases
- Functional Neurological Disorder (FND) Clinic – Provide intervention with patients with PNES, Functional Movement Disorders, Unexplained cognitive or vision changes
- Evaluation Clinic - Complete intake evaluations with families on BMH waitlist to determine service needs
Children's Integrated Care Team provides consultative and brief intervention services in the pediatric primary care clinic at Hughes-Spalding. The clinic serves a high proportion of children insured by Medicaid and is comprised of a team of pediatricians, medical residents and interns, psychiatrists, psychiatric nurse practitioners, psychologists, nurses, medical assistants, social workers, nutritionist, interpreters, and a growing team of behavioral and mental health therapists (LCSWs and LPCs). Interns can expect to provide brief behavioral and mental health consultations during patients’ medical appointments. Common presenting concerns seen in consultations include disruptive behavior, post-traumatic stress, autism spectrum disorder, ADHD, anxiety, and depression. Interns will also participate in follow-up visits focusing on brief, solution-focused interventions, either in conjunction with medical visits or during standalone behavioral and mental health visits. In addition, interns may participate in conducting expedited autism assessments for young children. Interns will participate in consultation and assessments with the supervisor initially and will gradually be given independence to conduct sessions as they demonstrate competency with the presenting concerns. Given the fast-paced nature of the Integrated Primary Care setting, the timeline will differ for each intern and each professional activity.
Due to the large and ever-growing number of Spanish-speaking families with behavioral health needs in our clinics, there are a variety of opportunities for bilingual (Spanish/English) training and supervision within the Behavioral Mental Health Track. Bilingual applicants are strongly encouraged to apply. There are bilingual supervisors as part of the BMH Outpatient Clinic and on the Integrated Care Team. There is the opportunity for specialized training in how to linguistically and culturally adapt Trauma-Focused Cognitive Behavior Therapy to working with Spanish-speaking families in our Trauma Clinic.
The Children’s Behavioral and Mental Health Outpatient Clinic and Integrated Care Clinic are relatively new, opening in 2021. This allows a unique opportunity for interns to gain experience in program development from both clinical and operational standpoints.
Interns will split their time between the Behavioral Mental Health Outpatient Clinic (Zalik location) and Integrated Primary Care at Hughes Spalding.
COMPLEX BEHAVIOR SUPPORT PROGRAM TRACK (1 position)
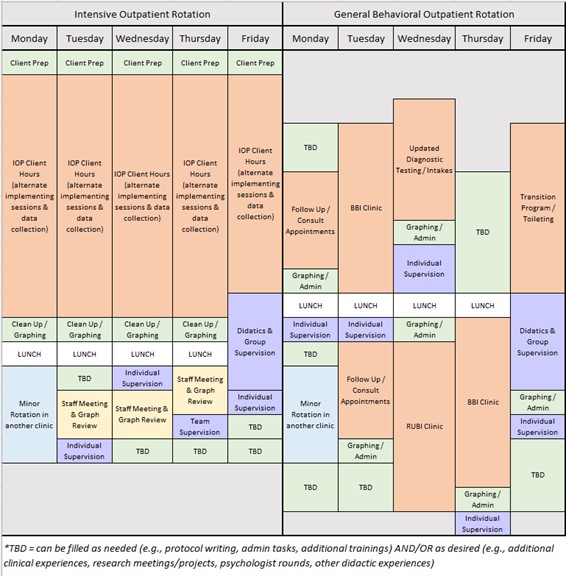
The Complex Behavior Support Program at the Marcus Autism Center provides a continuum of services for individuals with developmental disabilities between the ages of 2 and 21 years who display severe forms of externalizing behavior such as self-injurious behavior (SIB), aggression, property destruction, tantrums, elopement, pica and toileting incontinence. The primary goals of the program are to: (a) serve as a model for the evaluation and treatment of destructive behavior displayed by persons with developmental disabilities, (b) foster the development of new therapeutic procedures through systematic research, and (c) promote the effective application of empirically supported treatments through training and consultation.
The goal for each client is to decrease the occurrence of behavior that poses safety risks or interferes with their long-term quality of life. This process includes functional behavior assessment and evaluation of individualized intervention strategies. Therapeutic gains are systematically generalized to the client’s home environment, community, and school as relevant. Social and ecological validity of interventions is also a significant area of emphasis in all Complex Behavior Support programming and regularly reviewed as a department.
Four clinical services are available, with level of care matched to client and caregiver characteristics. Interns in the full-year Complex Behavior Support Program will spend half of the year in our Intensive Outpatient Program, which serves the most severe and complex behavioral cases in the region. Within this program, clients receive services for 5-hours a day, 5-days a week, for an average of 4 months. Individuals are referred to this program if their behavior is placing their family in a state of crisis (e.g., behavior is causing significant injuries or the family is considering residential placement for the individual) or if their behavior cannot safely be managed by the caregivers. Common service progression includes detailed functional analyses, teaching of adaptive behavior (e.g., functional communication training), identification of environmental accommodations, reinforcement for alternative behaviors on a dense schedule, schedule thinning, caregiver training, and generalization.
During the other half-year rotation in the Complex Behavior Support Program, interns gain experience providing a variety of less intensive outpatient type services. Interns will be matched to experiences based on interest as possible. Some examples of these outpatient services can include but are not limited to:
- Updated Diagnostic Testing: Conducting assessment appointments to update individual’s diagnoses to access behavioral services. These appointments often entail administration of caregiver completed measures, an autism specific clinician measure and semi-structured interview and observation of the individual and caregivers. These appointments are often conducted via telehealth with a licensed psychologist.
- Intakes: Conducting intake appointments to determine the appropriate referral for services in the Complex Behavior Support Program. These appointments entail structured interview and observation to determine level of care required. These are often conducted via telehealth and with a BCBA or licensed psychologist.
- Caregiver Psychoeducation: Conducting appointments in our RUBI Parent Training Program. This program uses a manualized intervention to support caregivers in addressing behaviors targeted for reduction. Each week involves teaching a new behavioral strategy that the parent is coached to implement. RUBI usually includes 12-15 hour-long appointments conducted weekly via telehealth with a licensed psychologist.
- Caregiver-mediated Behavioral Intervention: Conducting appointments in our Brief Behavior Intervention Program. This program works with clients whose behavior can be safely managed in a 1:1 context. Typically, appointments are twice a week for around a total of 5 hours with a BCBA and RBT. Some appointments are conducted via telehealth while some are in person.
- Short Term Follow Up: Coaching caregivers to continue to implement behavioral strategies with high integrity following a successful discharge from our Intensive Outpatient Program to ensure long term maintenance of skills.
- Toileting: Working 1:1 with a client to address toileting concerns using a systematic intensive toileting protocol.
- Transition Program: Working 1:1 with a client on skill acquisition and skill readiness protocols to ensure a successful transition back to school following a more intensive service admission.
- Hospital Consultation: Working with caregivers and health providers to provide general recommendations regarding environmental modifications and antecedent strategies to maximize safety and effectiveness of medical intervention for individuals with developmental disabilities within affiliated hospital settings.
Other Opportunities: There are various other types of outpatient appointments that could also be experiences including Consultation Appointments, Long Term Follow Up Appointments or even conducting sessions our Single Subject Research Laboratory.
INTENSIVE INTERVENTION TRACK (2 positions)
Interns in this track will spend 6 months in the Skill Acquisition Program and 6 months in the Multidisciplinary Feeding Program for a total of 2, 6-month major rotations.
The Multidisciplinary Feeding Program offers an intern the opportunity to work with children ages 9 months to 21 years who do not consume enough volume or variety of food to maintain adequate growth or nutrition. Children with this level of feeding disorder fall under the broader psychiatric diagnosis of Avoidant-Restrictive Food Intake Disorder (ARFID) or Pediatric Feeding Disorder (PFD). ARFID in pediatric populations or PFD often co-occurs with complex medical and/or developmental conditions (e.g., pre-maturity, gastrointestinal, cardiac, food allergy, autism); therefore, this rotation offers interns a breadth of training opportunities with a diverse range of patients. Our model of care involves multidisciplinary assessment and treatment and throughout the training year interns gain experience working with a team that includes physicians, nurse practitioners, dietitians, speech-language pathologists, an occupational therapist, and a social worker. Previous feeding experience is not required to apply for this position.
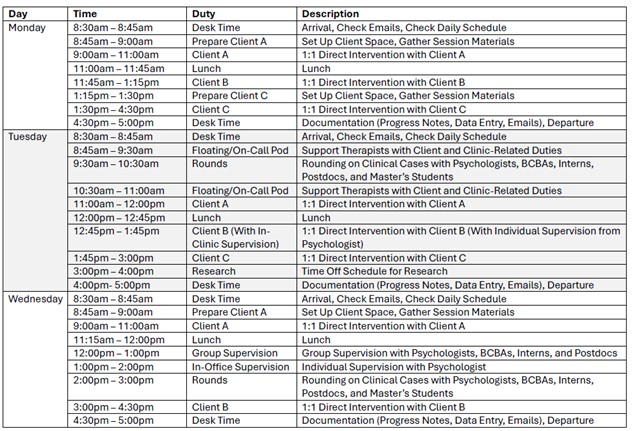
The Skill Acquisition Program at Marcus Autism Center serves children on the autism spectrum between the ages of 2 and 12 years (average 4 years of age) who are exhibiting significant language and social communication delays. Services provided focus on building communication skills, bolstering appropriate play and social skills, targeting foundational learning skills such as imitation and matching, and reducing barriers to learning (e.g., limited reinforcers, mild to moderate behavioral difficulties). The goal for each child admitted to the program is to acquire the critical skills they need in order to thrive in a less intensive setting. Children receive services between 3 and 6 hours per day, 5 days per week. All services are provided in a 1:1 format that utilizes a naturalistic developmental behavioral intervention (NDBI) approach to meet each child’s individual and developmental needs. Intervention also heavily involves caregivers via both didactic and in-vivo training to facilitate generalization, speed treatment progress, and support families holistically.
Interns in the Skill Acquisition Program have the opportunity to gain a diverse set of experiences that include working directly with children, providing consultation, and delivering caregiver training. They learn to conduct and utilize comprehensive language assessments to aid in the development of intervention programming that focuses on improving language skills, play skills, and adaptive skills and that addresses barriers that may interfere with learning. In addition, they learn how to integrate child development with evidenced-based practice in order to produce meaningful outcomes in the daily life of the children they work with. Interns will have opportunities to engage in multidisciplinary collaboration with clinical psychologists, board certified behavior analysts, registered behavior technicians, speech-language pathologists, nurse practitioners, and social workers. Interns will also have opportunities to participate in ongoing departmental research projects in the roles of designing and implementing research protocols, assisting with data collection and analysis, and manuscript writing.
MULTIDISCIPLINARY FEEDING PROGRAM TRACK (2 positions)
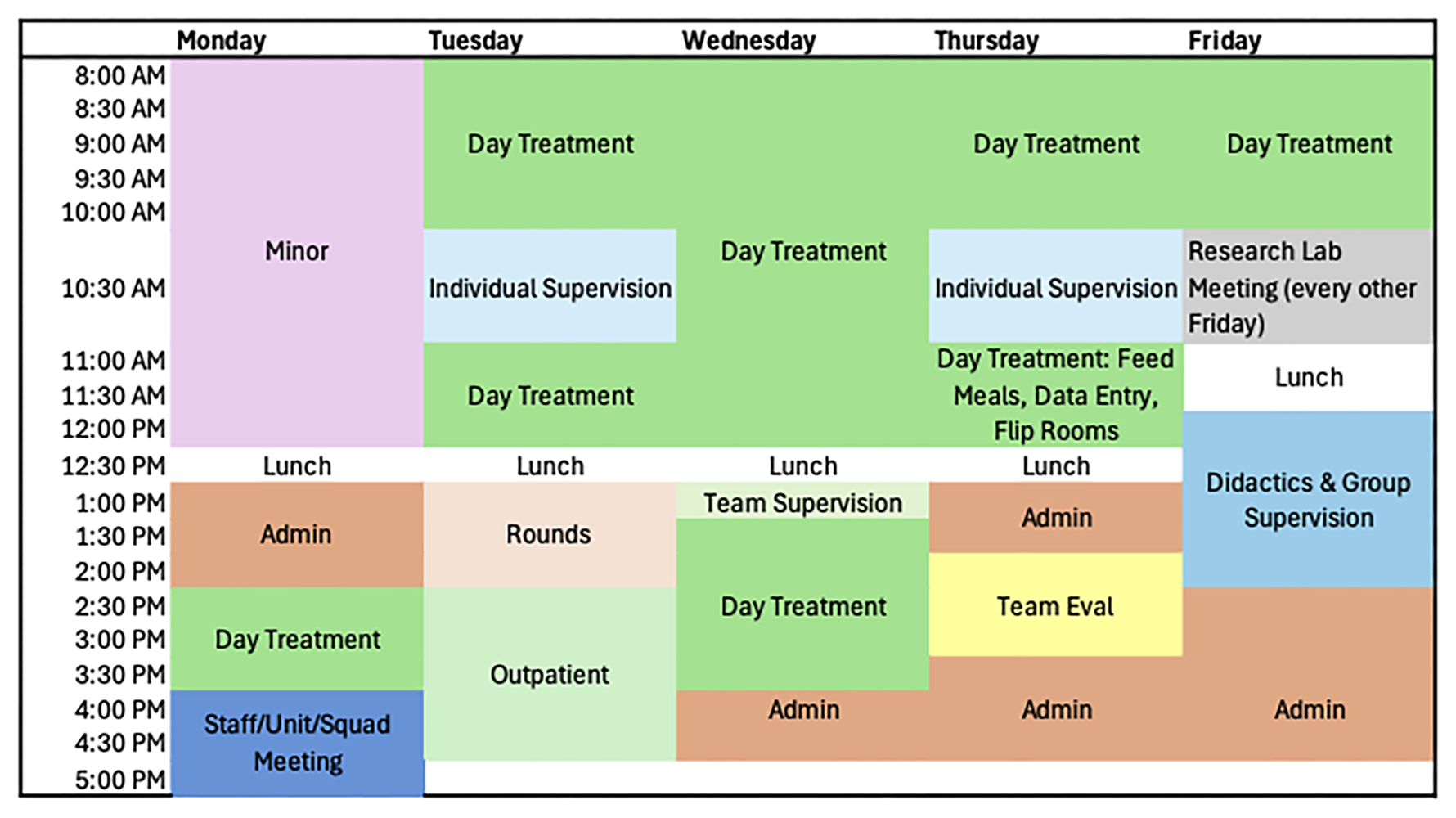
The Pediatric Feeding Track offers an intern the opportunity to work with children ages 9 months to 21 years who do not consume enough volume or variety of food to maintain adequate growth or nutrition. Children with this level of feeding disorder fall under the broader psychiatric diagnosis of Avoidant-Restrictive Food Intake Disorder (ARFID). ARFID in pediatric populations often co-occurs with complex medical and/or developmental conditions (e.g., pre-maturity, gastrointestinal, cardiac, food allergy, autism); therefore, this rotation offers interns a breadth of training opportunities with a diverse range of patients. Our model of care involves multidisciplinary assessment and treatment and throughout the training year interns gain experience working with a team that includes physicians, nurse practitioners, dietitians, speech-language pathologists, an occupational therapist, and a social worker.
The Pediatric Feeding Track offers a scientist practitioner model of training. Our clinic integrates science and best practices by involving a data-driven decision-pathway model of care that also facilitates new discoveries through single-subject research. The model of supervision is behavioral and involves competence-based benchmarks. The supervisor provides modeling and performance feedback with heavy oversight initially and support is faded as the internship progresses.
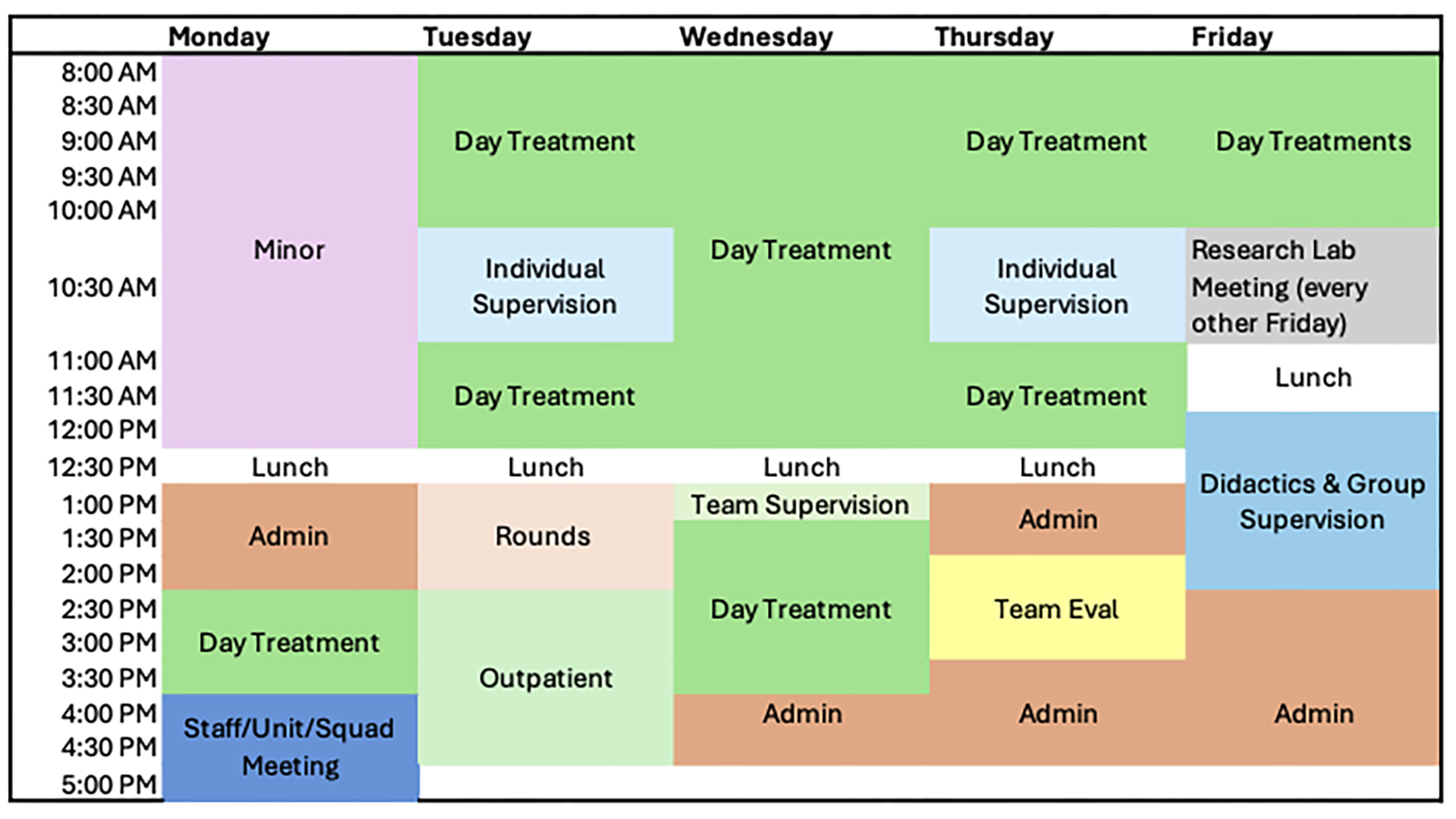
The intern in the Pediatric Feeding Track will spend a full year training in clinical experiences that include feeding assessments, intensive day treatment, and outpatient therapy. Across these areas, interns will gain experience with treatment approaches that include applied behavior analysis, parent training, parent-child interaction therapy, and manual-based interventions. Interns will split their time between Marcus Autism Center, the Center for Advanced Pediatrics, and community outpatient settings. In addition to feeding, treatment often focuses on associated behavioral/pediatric concerns including sleep, toileting, and disruptive behavior. Professional opportunities include participating in grant funded and/or clinical research projects, presentations at regional and national conferences, and supervision of others.
NEURODEVELOPMENTAL ASSESSMENT AND EARLY INTERVENTION TRACK (2 positions)
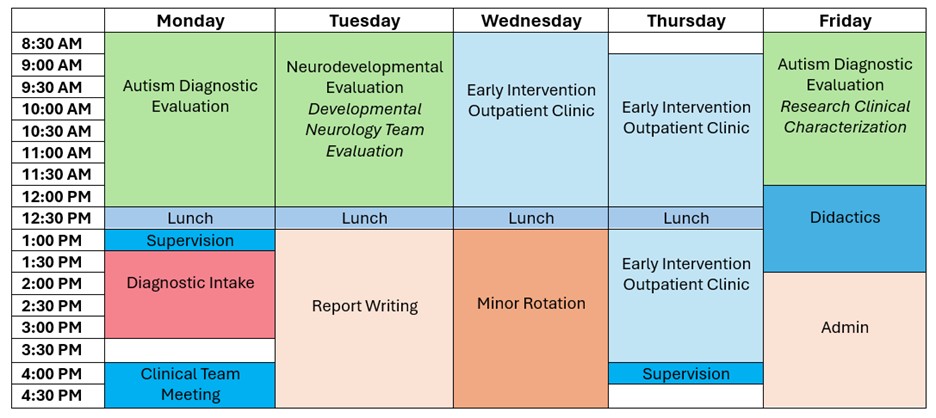
Interns in this track split their time between two year-long major rotations with the Clinical Assessment and Diagnostics (CAD) Department and Project ImPACT Early Intervention (EI) Clinic at the Marcus Autism Center, with options for minor rotations in other CHOA clinics. These major rotations offer a shared focus on early identification of and supports for neurodevelopmental disorders as well as family engagement and empowerment. Families served represent diverse ethnocultural, racial, linguistic, and socioeconomic backgrounds, and most families qualify for state or federal Medicaid. An example of how interns may split their time each week is: 1 day in the EI Clinic, 2 days in CAD, as well as time committed to a minor rotation and administrative commitments, follow-up client care, and training commitments like didactics.
CAD emphasizes flexible, empirically supported approaches to clinical assessment with an emphasis on family-centered care. Within half- and full-day diagnostic assessments, interns support individuals ranging from infancy to late adolescence with a range of neurodevelopmental disorders, all with a presenting diagnostic question of autism. Although we serve a full age range of clients from 12 months to 18 years, most children seen are ages 5 and under. Children are commonly assessed for autism spectrum disorder as well as common differential diagnoses such as intellectual disability, language disorders, anxiety disorders, and ADHD. Assessments are designed to identify cognitive and developmental strengths and areas of challenge, assess adaptive functioning, provide diagnostic clarification, and aid families in identifying and accessing community-based supports. There are opportunities to join psychologists for evaluations across various research studies as well.
Assessment teams often consist of one psychologist working alongside an intern or postdoctoral fellow, with opportunities to consult with related professionals. Located alongside our clinic are psychiatrists, nurse practitioners, speech language pathologists, and social workers. Interns may also join psychologists conducting multidisciplinary evaluations with developmental behavioral pediatricians and neurologists. Interns will have the opportunity to participate in assessments that include interpreters and, for interested trainees proficient in Spanish, bilingual assessments, interventions, and supervision is available.
EI uses an outpatient parent coaching model to support families of autistic toddlers or those with social communication delays. EI centers on the evidence-based Project ImPACT curriculum while also supporting families in navigating barriers to care. The program emphasizes family engagement by coaching families on how to implement developmental and behavioral teaching strategies across daily routines and then creating plans for weekly practice. Children seen range from 12 to 40 months and demonstrate varying degrees of social and communication delays (e.g., skills ranging from limited vocal and gestural communication to speaking in short sentences with challenges engaging with others). Presenting concerns include autism but also language disorders, genetic disorders, cerebral palsy, and factors associated with preterm birth.
With respect to intern supervision across the EI and CAD major rotations, all psychologists are a part of the same team, with many working in both CAD and EI. Supervisors have broad training in clinical psychology with experience working with pediatric populations with and without autism. Supervisors generally ascribe to a cognitive behavioral theoretical orientation. CAD and EI supervisors place high value on training and enjoy working closely with trainees from varied backgrounds.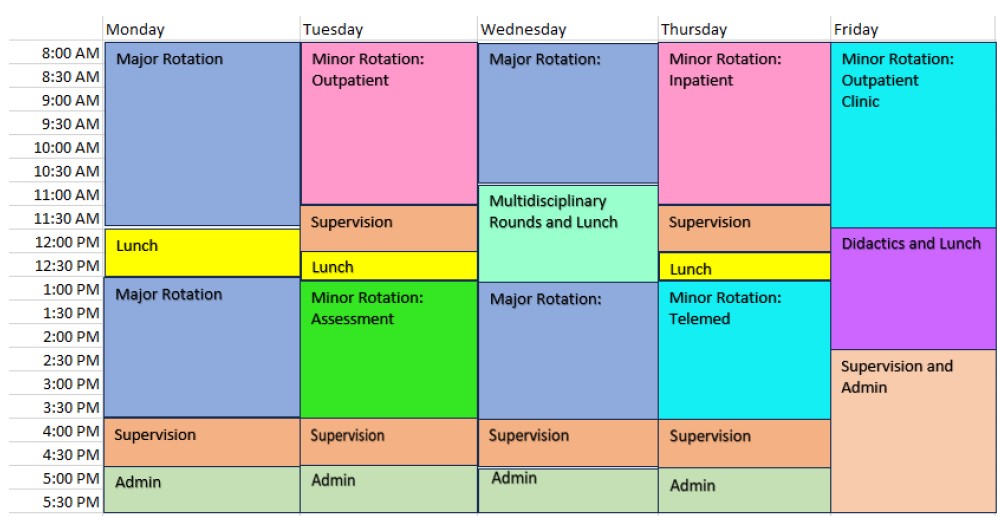
PEDIATRIC PSYCHOLOGY TRACK (2 positions)
The Pediatric Psychology Track offers an intern in-depth training in pediatric psychology. The Track teaches interns assessment, treatment, and consultation skills for youth presenting with co-occurring medical and psychological problems. Skills are developed across a continuum of care settings including: 1) clinic-based consultation, assessment, and intervention, and integrated care pediatric psychology, 2) inpatient pediatric psychology, and 3) consultation-liaison services across multiple medical specialties. Across settings, interns gain experience in multidisciplinary and interdisciplinary care of behavioral and medical problems. Focus is placed on learning to implement different models of psychological assessment and intervention in integrated care settings. Interns have the opportunity to maintain long-term treatment cases. Behavioral and cognitive-behavioral interventions are the primary treatment modalities, with emphasis on a family systems perspective.
Specific rotations may vary each year, but for the 2026-2027 training year, pediatric psychology rotations include outpatient, clinic-based consultation, and integrated care with the following patient populations: gastroenterology, endocrinology, sleep disorders, solid organ transplant, cardiac neurodevelopmental assessment, complex headache, complex concussion, and differences in sex development. Additionally, inpatient and intensive pediatric psychology rotations will be available in cardiology, solid organ transplant, palliative care, and rehabilitation.
Interns engage in two, six-month major rotations: 1) Rehabilitation and 2) Cardiology and Solid Organ Transplant, as well as 3-5 minor rotations per six-month period.
Professional opportunities include participating in grant-funded and/or clinical research projects, giving presentations at regional, national, and international conferences, engaging in community advocacy, and supervising externs.
POSSIBLE MINOR ROTATIONS
Interns in all tracks participate in a ½ day a week Minor Rotation. Most minor rotations are 6-month experiences, allowing for broader experience across the training year. Some minors requiring highly specialized training are scheduled for the full year. Minor Rotations are determined after the match. Possible minor rotations are listed below. The availability of minors varies from year to year.
Behavior Mental Health Evaluation Clinic (minor rotation) offers interns the opportunity conduct initial outpatient evaluations for children ages 4-18 years old to determine needed outpatient services (i.e., therapy, psychiatry). Patient concerns include anxiety, depression, disruptive behavior, ADHD, OCD, and trauma. Many patients have comorbid medical conditions and are referred from endocrinology, oncology, neurology, transplant, and orthopedics.
RUBI-Parent Training Program (minor rotation) within the Severe Behaviors Program is an outpatient program developed and shown to decrease challenging behaviors in children with an Autism Spectrum Disorder (ASD) between the ages of 3 and 10. The program involves teaching parents a number of strategies to prevent, manage, and reduce occurrences of problem behaviors of mild to moderate severity while promoting skill development.
The Brief Behavior Intervention (BBI) Program (minor rotation) is a weekly outpatient program. Children have a variety of problem behaviors of moderate to high severity, including aggression, self-injury, noncompliance, disruptive behavior, elopement, and pica. Targeted treatment goals are achieved through the therapist coaching the caregiver in completing a functional analysis and implementing treatment. There is a heavy emphasis on parent training, with the caregivers rehearsing skills both during the appointment as well as between appointments. ABA experience is required.
The Clinical Assessment and Diagnostic Department (minor rotation) is a multidisciplinary clinic that provides diagnostic assessments of individuals with a wide range of neurodevelopmental disorders with a possible autism spectrum disorder. Children seen in the CAD clinic range from infancy to late adolescence with a focus on children ages 16 months to 6 years.
The Cognitive Behavioral Therapy for Anxiety/ASD (minor rotation) is 12-20 weekly individual therapy sessions with utilizing Facing Your Fears (e.g., emotional identification and awareness, exposure exercises, role modeling, using tech to integrate their strong interests, coping skills) Clients must be at least 10Y+ with average or above average IQ. Treatment will also include 3-week social skills module and weekly parent sessions. Individual therapy experience required.
The Early Intervention Program (minor rotation) is an outpatient 12- to 15-week naturalistic developmental behavioral intervention to help caregivers of children under the age of 42 months with social communication delays develop their children's play and communication skills. The program centers on the Project ImPACT parent coaching curriculum, which integrates behavior analytic techniques with child-led developmental strategies. Sessions take place once each week for one hour. Previous experience with parent coaching models preferred. BCBA supervision hours are not available for this rotation.
The Multidisciplinary Pediatric Feeding Clinic (minor rotation) offers interns the opportunity to work with children ages 9 months to 21 years who do not consume enough volume or variety of food to maintain adequate growth or nutrition. Children with this level of feeding disorder fall under the broader psychiatric diagnosis of Avoidant-Restrictive Food Intake Disorder (ARFID).
The Neuropsychology Clinic (Minor open to Clinical Assessment and Diagnostics/Early Intervention Track Interns ONLY) involves conducting psychological evaluations under the supervision of board-certified neuropsychologists in CHOA’s neuropsychology program. Presenting concerns include TBI’s, genetic disorders, seizure disorders, or chronic illnesses associated with neurocognitive deficits.
Pediatric Psychology (minor rotation) – Significant therapy experience and familiarity with medical populations required.
- Inpatient Rehabilitation- Assessment, consultation, and intervention on 27-bed inpatient pediatric rehabilitation unit on the Scottish Rite campus. Working with patients with diagnoses requiring intensive Occupational, Physical and Speech Therapies including traumatic and acquired brain injuries, spinal cord injury, and complex medical conditions.
- Sleep - The sleep rotation will focus on outpatient treatment of patients from infancy through young adulthood who are primarily presenting with insomnia or difficulties with adherence to CPAP using behavioral/cognitive behavioral interventions.
- Solid Organ Transplant - Consultation-liaison assessment and intervention with children and adolescents who have received kidney or liver transplants.
- Complex Headache - Complex Headache Clinic is a multidisciplinary outpatient clinic through the Department of Neurology that evaluates and treats children and adolescents with various headache disorders (e.g., chronic migraine, new daily persistent headache) that have persisted for more than 1 year or have failed to respond to several medical interventions.
- Gastroenterology - The gastroenterology rotation will focus on outpatient treatment of patients from early childhood through young adulthood presenting with a variety of gastrointestinal conditions including irritable bowel syndrome, rumination syndrome, dysphagia, inflammatory bowel disease, and constipation. Treatment will primarily include cognitive-behavioral approaches. Depending on the day of the rotation, there may also be opportunities for inpatient work and multidisciplinary outpatient clinics.

