Infection Control System for Resuscitation and Airway Management

This collapsible, single-use 'pop-up tent' system was created to prevent transmission of infectious disease to providers and staff members during patient resuscitation and intubation/airway management (pictured). This system provides a pliable, translucent barrier between the patient and medical staff, while allowing visibility and access to the patient for airway procedures. The multidisciplinary design team consists of Adam Klein, MD, director of the Emory Voice Center; Russell Gore, MD, director of vestibular neurology at Shepherd Center; and David Wright, MD, chair of the Emory Department of Emergency Medicine. The device is in the prototyping stage.
Compositions of Transforming Growth Factor-Beta Type III Receptor and Uses for Ossification
International Patent No. WO 2019/236837 A1
Developed by Steven Goudy, MD, director of pediatric otyolarngology at Children's Healthcare of Atlanta, this bone regeneration approach can be used to improve bone formation after surgery to repair a bone void such as an orofacial cleft, cleft palate, or cleft lip.
Nasal Suction Device

U.S. Patent No. 10398810
Dr. Steven Goudy collaborated with doctoral students, researchers, designers, and families to create The NozeBot, a hospital-quality, vacuum-powered, safe, and hygienic solution for clearing infants' nasal passages that is easy for parents to use either at home or while on the go.
PhonoSurgical Trainer

U.S. Patent No. 8647125 B2
The PhonoSurgical Trainer is an educational tool for otolaryngologists, laryngology fellows, otolaryngology residents, and medical students to aid in the proficiency of phonomicrosurgery and other phonosurgical procedures. The system was designed by Dr. Adam Klein in collaboration with other surgeons and industry to ergonomically simulate actual cases in an operating room setting, and offers cost-effective disposable vocal folds that allow the user to practice at their convenience without dependence on the availability of cadaveric, porcine, or bovine specimens.
Phonomicrosurgical Arm Support

U.S. Patent No. D0728800
Dr. Adam Klein developed this surgical wrist support device to aid surgeons in performing microsurgeries, such as phonomicrosurgery, though it may also be used for any procedure involving fine hand movements or that requires surgeons to hold their arms or hands in position for extended periods of time. The device is intended to reduce tremors in the physician's hands, reduce surgery time, and potentially improve patient outcomes.
Ventilated Upper Airway Endoscopic Endonasal Procedure Mask
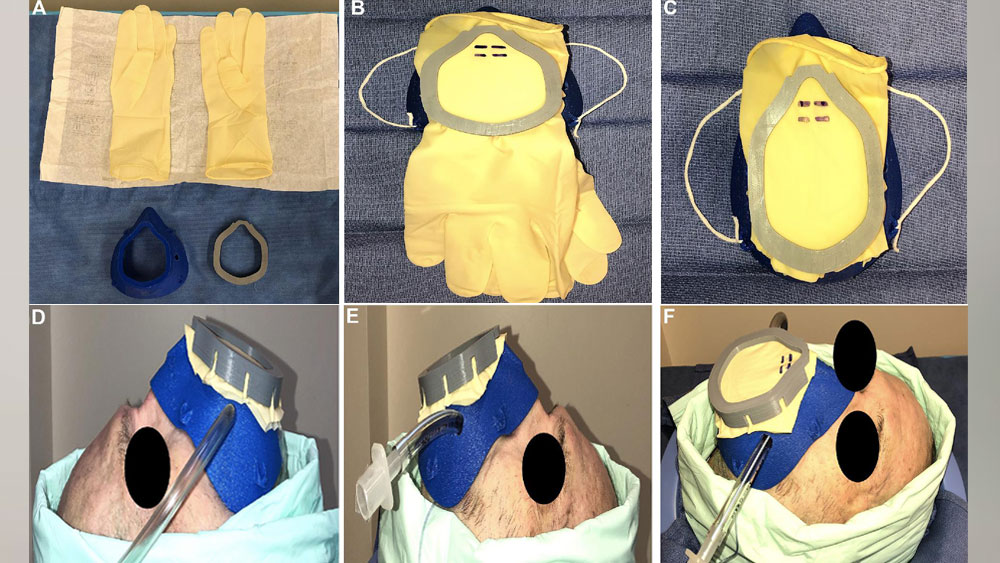
The Ventilated Upper Airway Endoscopic Endonasal Procedure Mask (VPM) was developed by Samuel N. Helman, MD, associate member of Emory Otolaryngology, in collaboration with Emory skull base surgeon C. Arturo Solares, MD, and Georgia Institute of Technology faculty Vahid Serpooshan, PhD, and Martin Tomov, PhD. The VPM is designed to protect otolaryngologists and their surgical teams from particle aerosolization during the COVID-19 era. Dr. Helman is working with Dr. Solares, Dr. Adam Klein, and additional Emory Otolaryngology members Joshua Levy, MD, Sarah Wise, MD, and John DelGaudio, MD, on the deployment of the VPM mask during real-life surgical and in-office encounters.
3d-Printed Tracheal Splint
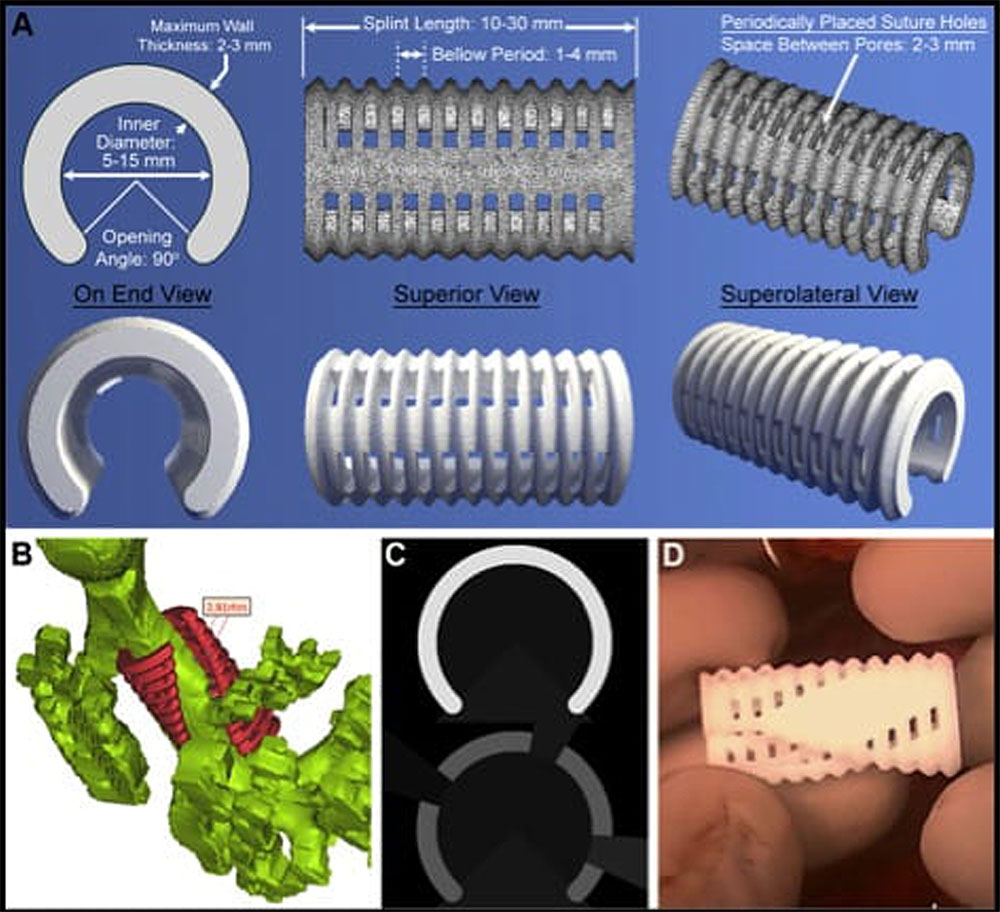
The 3d-printed tracheal splint was designed and developed by Scott Hollister, PhD, and his team at the Tissue Engineering and Mechanics Lab at Georgia Technology Institute. The device is intended to battle life-threatening airway obstruction, and has been implanted in several pediatric patients at Children's Healthcare of Atlanta by a multidisciplinary team led by Dr. Steven Goudy and his Emory Otolaryngology colleague April Landry, MD.
The splints are designed using reconstructions of patients' airways from CT scans, printed as porous scaffolds by the Global Center for Medical Innovation, and placed around patients' tracheas by the surgical team. After implantation, the splints are eventually absorbed into the body, allowing for expansion of the trachea and bronchus.
Visit the Dr. Hollister-directed Tissue Engineering and Mechanics Lab at Georgia Tech
11 Alive News Story on the use of the tracheal splint in a pediatric surgical procedure
Theranostic Biomarker for Aspirin-Exacerbated Respiratory Disease
Joshua Levy, MD, MPH, and Samuel Molina, PhD, have identified biomarkers for a non-invasive clinical diagnostic tool and non-psychogenic therapy to detect and treat aspirin-exacerbated respiratory disease. This method does not rely on aspirin challenge, thereby increasing safety and availability for prospective patients, and could be used in patients who have respiratory compromise or are not stable.
In addition to being a faculty member of Emory Otolaryngology, Dr. Levy is also a member of Michael Koval's laboratory at Emory University School of Medicine.
Emory Office of Technology Transfer description, patent pending

