Improving Care for Tomorrow
-
Vision
-
To use innovation, education, and discovery to improve the care of critically ill children
-
-
Mission
-
Train the next generation of academic leaders in pediatric critical care
-
-
Values
-
Mentorship central – constant, personalized, and developmental
-
Optimize and balance the training paradigm – development of dual expertise
-
Fellow Forward – placing trainees into a position of success
-
Lifelong Inquiry – an extension of learning, asking questions now and beyond
-
Engagement, Enjoyment, and Enthusiasm – fellowship research redefined
-
Timeline
Research goals
-
Prior to Arrival: Brainstorm and Mapping
-
Year 1
-
Months 1-3: Thought funnel, initial meetings
-
Months 4-6: Formation of a Mentorship Team
-
Months 6-12: Development of Primary Research Project
-
-
Year 2
-
Engagement and ownership of project follow through
-
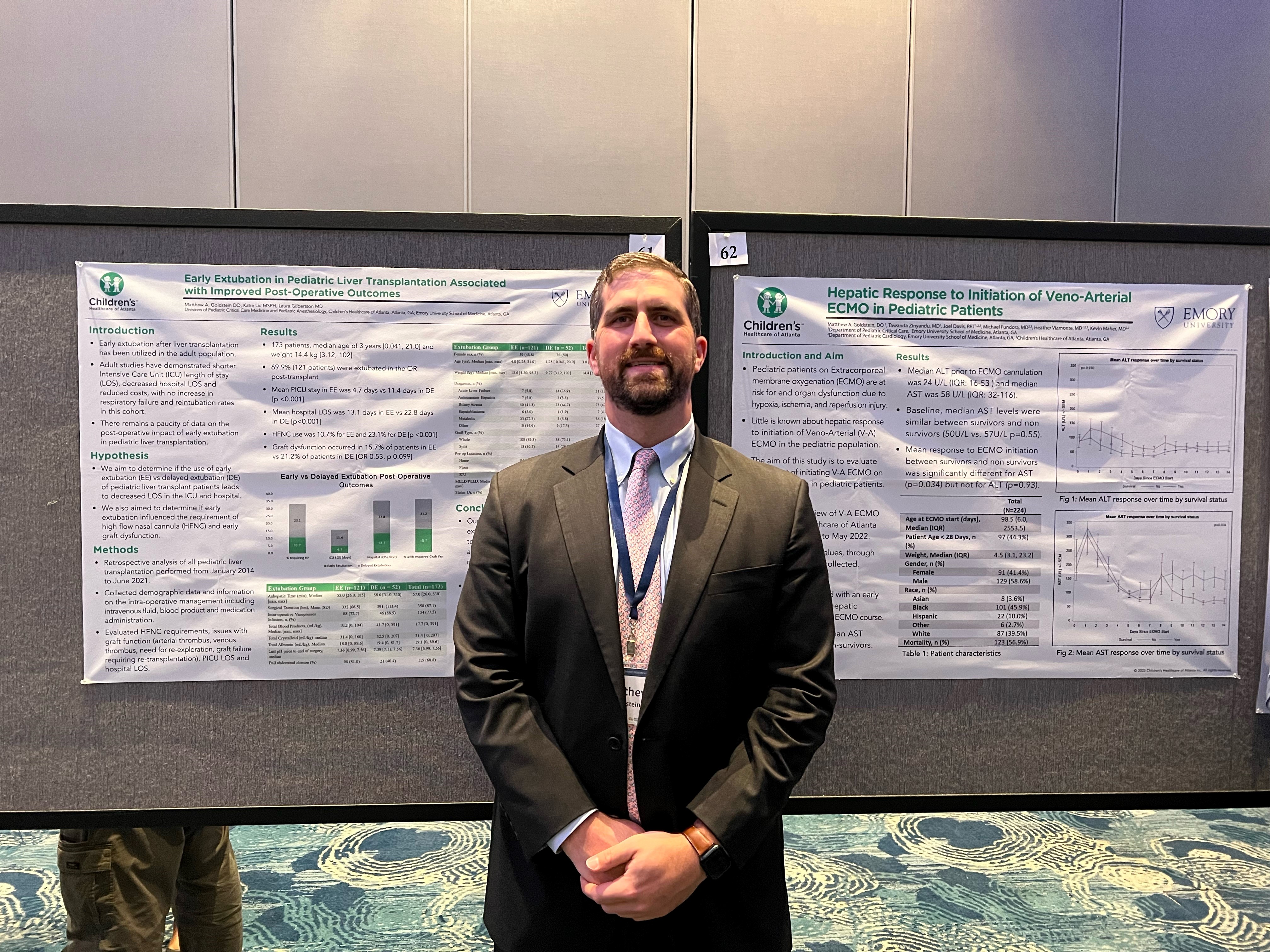
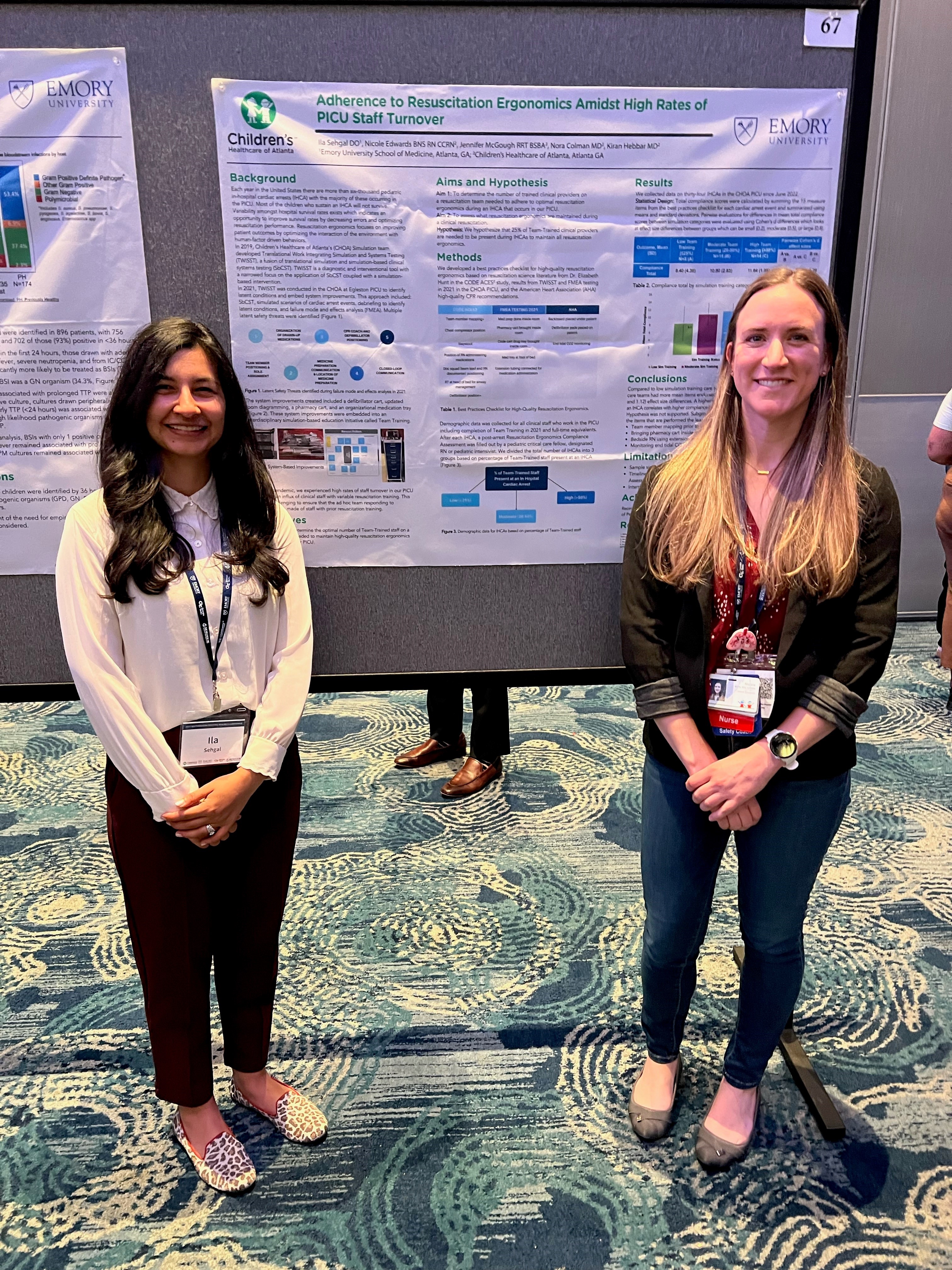
Initial results and presentation at national meeting(s)
-
-
Year 3
-
Finalization of primary project
-
Secondary project(s)
-
Development of Junior Faculty Research Map
-

Recent Fellow Projects
TBI and Presenting HTN
Automated Pupillometry and ICP
ECMO and Redox Potentials
ECMO for massive Pulmonary Embolism
Sedation Trend Analysis - Protocol Change
Unplanned Extubation - Compliance and Rate
Fluid Overload Kinetics and Outcome
Resource Utilization in Pediatric Poisonings
A Phenotype Derivation of Burnout
Early Mobility Implementation - A QI Analysis
Cirrhotic Cardiomyopathy Epidemiology
Cerebral Oxygen Metabolism and Sedation
Intubation Checklist and Team Training
Rapid Cycle Practice in Shock Management
Adverse Childhood Experiences in Critically Ill Children
Predictive Factors for Successful Discontinuation of CRRT
Immune Phenotyping in Pediatric ARDS
Ultrasound Imaging of Endotracheal Tube Positioning
Sedation Protocol in Patients Undergoing MIBG Therapy
Outcomes of Children with Life-Threatening Asthma
Neighborhood Hot Spots in Acute Respiratory Failure

Collaborative Research