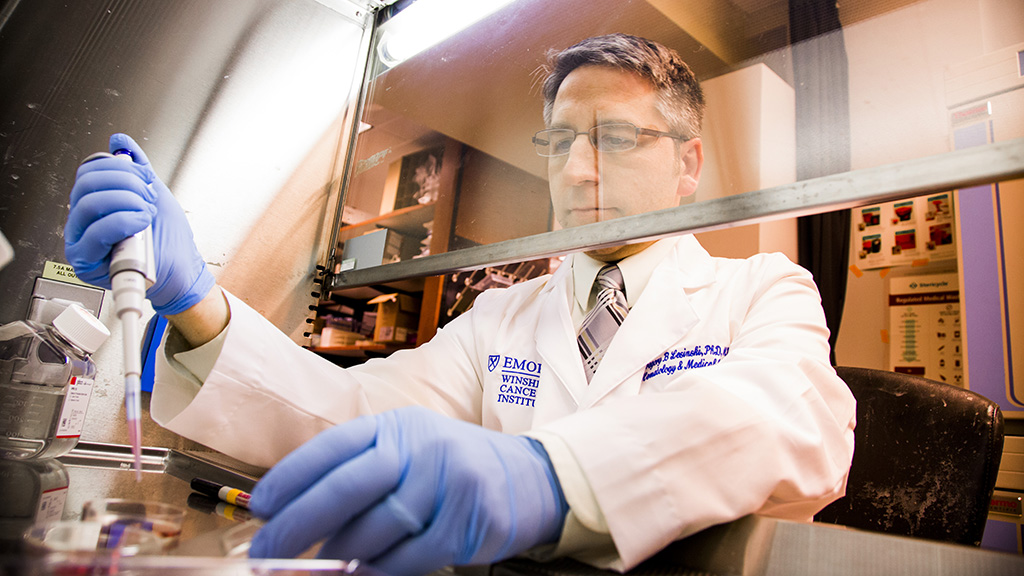
Translating novel immune and targeted therapies
Our translational research team has studied a variety of solid tumor malignancies including pancreas, liver (biliary, HCC), melanoma, head and neck cancer and prostate cancer.
Our laboratory has also served as the lead site for correlative studies associated with several solid tumor oncology clinical trials over the last several years. Of over 105 publications total, 39 involve human samples, 17 of which involve Phase I clinical trials, or key pre-clinical data that led to these trials. Many studies represent first in man combination therapy against cancers, including pancreatic cancer where correlative studies for these trials took place in our laboratory. Our group thrives on collaborative integration with clinical investigators in a multi-disciplinary setting. Our group has made advances in understanding complex interactions between tumors, stroma and the immune system, adapting novel immunotherapy combinations from the lab into the clinic, and in limiting chronic inflammation as a mediator of carcinogenesis.
Our overall goal is to maintain a highly-collaborative research program focused on translating novel immune and targeted therapies into clinical trials for patients with gastrointestinal and other solid tumor malignancies. Our focus has been to pursue combined therapeutic approaches targeting cytokines and signaling pathways derived from the tumor and stroma to enhance the efficacy of immunotherapy. Of particular interest will be signal transduction pathways that have a shared role in promoting tumor cell growth or metastasis and immune suppressive cell expansion.
Priority research areas
To determine how targeting the stromal components of gastrointestinal cancers can be leveraged to enhance immunotherapy, and translate them into clinical trials.
Our laboratory is expanding on our prior observations that IL-6 is a poor prognostic indicator in patients with metastatic pancreatic cancer (Farren et al., Clin Cancer Res, 2016) and may be derived from tumor stroma as a means to facilitate immune evasion by the cancer (Mace et al., Cancer Res, 2013). Further research showed that targeting IL-6 and the PD-1/PD-L1 immune checkpoint led to T cell dependent anti-tumor efficacy in a variety of murine pancreatic cancer models (Mace et al., Gut, 2016). Studies funded by an NCI R01 grant (PI: Lesinski; 1R01CA208253-01) have focused on delineating the mechanism for anti-tumor efficacy in vivo and understanding how IL-6 blockade can be further leveraged to enhance efficacy of immunotherapy. This work has translated into a first in human Phase Ib/II clinical trial of dual IL-6/PD-1 blockade that is ongoing (Clinical Investigator: Maria Diab). Importantly, we are using clinical samples from this trial to better understand the impact of the regimen on both cancer associated fibroblasts and immune features in the context of a funded NCI R21 grant (MPI: Lesinski, El-Rayes, 1R21CA266088-01).
This work complements other observations from our group in collaboration with Bassel El-Rayes at University of Alabama, Birmingham that heat shock protein-90 (Hsp90) represents an inflammatory pathway in pancreatic cancer associated fibroblasts that can be inhibited together with PD-1 blockade to limit pancreatic tumor progression (Zhang et al., Mol Cancer Ther, 2020). This work also led to an NCI R01 grant (MPI: Lesinski, El-Rayes, 1R01CA228406) that will further define the mechanism of this therapy in both pre-clinical models and in samples from patients receiving this combination as part of an early phase clinical trial.
In collaboration with Chrystal Paulos, we are evaluating the role of other proteins including DPP4/CD26 expressed on multiple cell types that influence immunotherapy response in pancreatic cancer (PI: Lesinski, Morningside Foundation). We continue an ongoing collaborative relationship with clinical investigators in Pathology, Surgery and Medical Oncology that can facilitate this research to discover new therapeutic targets and validate previously identified genes and pathways within the stroma. The role of the stroma in carcinogenesis is quite complex, and these studies will add to our understanding into the dynamic process that occurs within the tumor microenvironment.
To develop and translate novel immunotherapy approaches for patients with advanced solid tumors.
Given the redundant factors that suppress T cell-mediated anti-tumor immune responses, we posit that combinatorial therapeutic approaches are needed to provide lasting efficacy in many patients, particularly those with immunologically cold or immunotherapy resistant tumors. Our team is actively engaged in several collaborative projects that take an aggressive approach to combination immunotherapy for advanced cancer and explore new bold approaches in the laboratory that may ultimately translate into early phase clinical trials for patients.
First, our laboratory has actively collaborated with Drs. Nilofer Azad and Mark Yarchoan at Johns Hopkins University to introduce immune checkpoint blockade in combination with MEK inhibition for patients with advanced biliary tract cancers. This work led to an NCI-funded R01 grant (MPI: Azad, Lesinski, 1R01CA228414) that supported correlative studies from a national, phase II clinical trial that was recently published (Yarchoan et al., JCI, 2021). Further laboratory studies detailed how this regimen can be improved upon through incorporation of T cell agonistic antibodies (Dennison, Cancer Immunol Res, 2021), which is now being explored in a second national, phase II clinical trial targeting PD-L1 and CD27 alone vs. PD-L1, CD27 and MEK signaling. This work complements our ongoing collaboration with Shishir Maithel, Alyssa Krasinskas and Brian Robinson in understanding factors that contribute to poor immunotherapy response in biliary tract cancers (Ware et al., Br J Cancer, 2020) and identifying new therapeutic targets for these patients.
Second, our laboratory is engaged in exploring novel agents that act upon myeloid cells to enhance the efficacy of T cell based immunotherapy in solid tumors. This work is being done in close collaboration with the laboratories of Brian Olson and Chrystal Paulos. Of particular interest is targeting the semaphorin 4D (SEMA4D) protein and its interaction with plexin receptors, which regulates immune cell trafficking into tumors. Our laboratory is involved as a lead site for correlative studies for clinical trials with pepinemab, an antibody targeting SEMA4D in melanoma (Clinical Investigators: Michael Lowe, Ragini Kudchadkar, Keith Delman) and head and neck cancer (Clinical Investigators: Conor Steuer, Nabil Saba).
Third, we are working closely with Mehmet Akce to understand how applying the combination of the multi-tyrosine kinase inhibitor, regorafenib with PD-L1 blockade in the pre-operative setting can benefit patients with hepatocellular carcinoma and modulate key immune features within these tumors. Finally, in collaboration with Edmund K. Waller and Chrystal Paulos we are exploring novel adoptive cell therapy approaches for advanced pancreatic cancer to further our arsenal of therapies against this disease.