For the Image of the Week this week we trying something a bit different. Have you ever struggled to manage headaches in the ED? If so, learning how to obtain the image below may help you!
Ultrasound-Guided Occipital Nerve Block: A How-To Guide
The situation: an elderly female with numerous medical problems, multiple medication allergies, and a history of chronic migraine presents to your emergency department with a headache typical of her usual migraines. The headache starts at the base of her skull and radiates forward, throbbing behind both eyes. There are no concerning historical details and no significant findings on physical exam. The patient is tearful, stating that when she had her last severe migraine several months ago she had to be admitted to the hospital for pain control. It is her granddaughter’s first birthday party the following day, and she will be heartbroken to miss it. You scratch your head, stare at her past medical history and allergy list, and contemplate your options. Her chronic kidney disease, heart failure, and history of prolonged QTc prevent you from using your standard migraine cocktail, and opioids are a poor choice of treatment for most headaches. When you see the ultrasound machine faithfully sitting in the corner, the answer comes to you: an ultrasound-guided occipital nerve block.
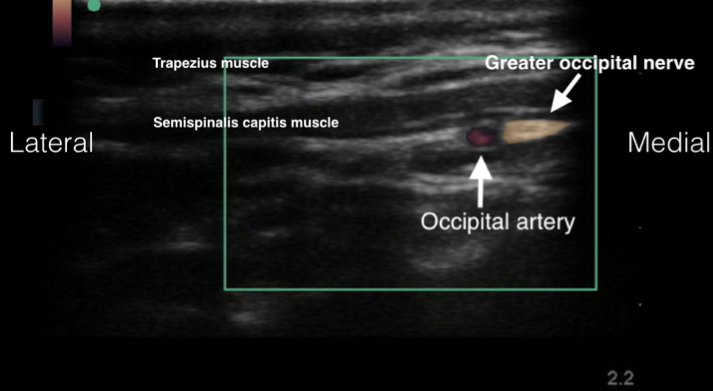
A greater occipital nerve block can provide quick and prolonged pain relief for patients suffering from cervicogenic headaches, occipital neuralgia, and cluster headaches. There is some evidence to support the use of this block in NSAID overuse and tension-type headaches. It is thought that the greater occipital nerve can become entrapped or inflamed at the areas on the skull where the trapezius and semispinalis capitis muscles attach to the occipital bone.
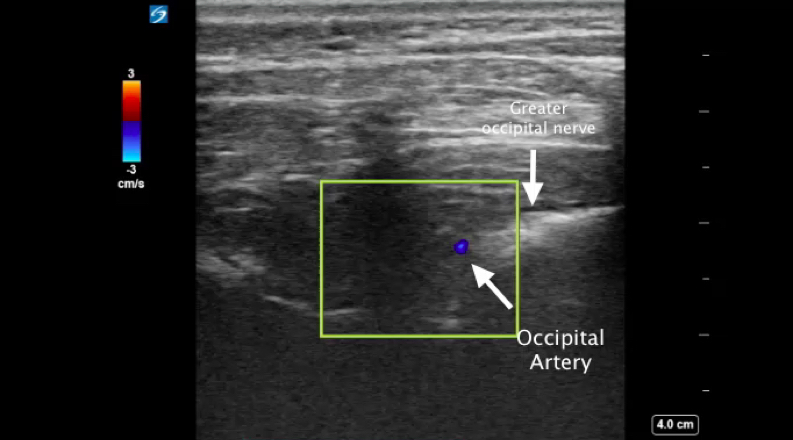
The procedure is simple to perform. The patient can be positioned sitting up with the head flexed slightly forward, or lying in the prone position. The occipital artery is found by palpating along the superior nuchal line until you locate the pulsating artery, normal about 3cm lateral from the inion. The greater occipital nerve should be running medial to the artery.
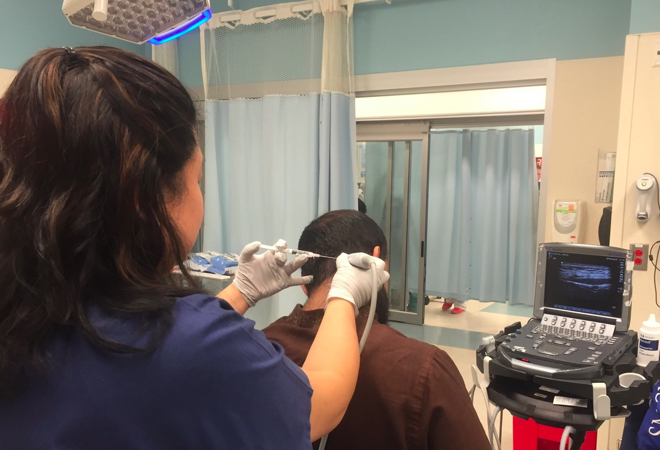
To do this procedure under ultrasound guidance, place the linear probe in a transverse orientation over the superior nuchal line lateral to the inion. You will be able to identify the pulsating occipital artery and can utilize color flow Doppler for confirmation. You should then be able to locate the greater occipital nerve as a white bundle medial to the artery.
Inject one to three milliliters of either 1% lidocaine or a 50/50 1% lidocaine/0.25% bupivacaine mixture above the nerve, taking care to avoid injecting directly into the nerve fascicle. The patient should have a quick improvement in their pain. Some studies have shown that patients can have prolonged improvement in their pain up to four weeks after the procedure.

