There was an epidemic of unilateral vision loss in the ER this week! Our IOW comes to us from Hiren Patel, Brooks Moore, Kristina Hester, Gina Porter, Brent Allen, and Anne Daul, who all successfully used ultrasound to diagnose retinal detachments in different patients. If you are like me the image below of a retinal detachment might as well be a figment of your imagination. The fundoscopic exam is challenging in an undilated ER patient. Small retinal flaps are often subtle, and ultrasound provides a great alternative for diagnosing this vision-threatening emergency.
Image 1
 .
.
Patients with a retinal detachment can present with flashers and floaters or can describe the classic loss of vision in a curtain-like distribution. They can occur spontaneously or following trauma, often delayed days or weeks after the inciting event. It is important to distinguish whether the detachment involves the macula, with loss of central vision, as these patients require emergent ophthalmologic intervention to preserve vision. To do this exam, really pile on the gel to make the exam more comfortable and avoid putting too much pressure on the eye. Bracing your palm on the patient's nasal bridge can also help with this. You can cover the eye with Tegaderm to avoid a goopy mess. Once you have visualized the eye you can over-gain the image to make structures in the posterior chamber more prominent, or have the patient move the eye to help you visualize a detachment that may appear to float back and forth as the eye moves.
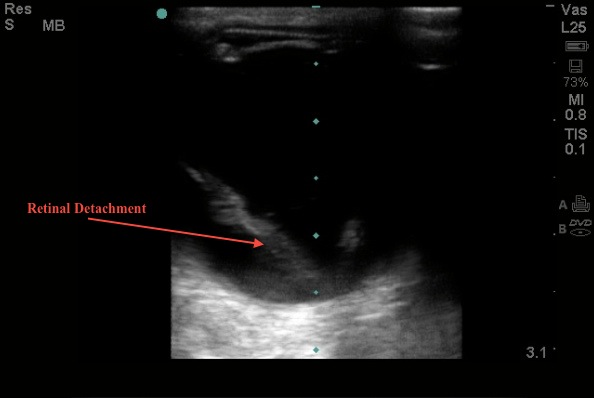
These ultrasound images each show different retinal detachments. A detached retina will ultimately tether to the optic nerve and the ora Serrata (the junction of the iris and the retina), but smaller flaps may not reach these landmarks. Remember all patients with vision loss need close ophthalmologic follow-up, so interpret your ultrasound in the context of the patient presented as a whole. It is probably a better test to rule in disease than to rule it out.
Image 2
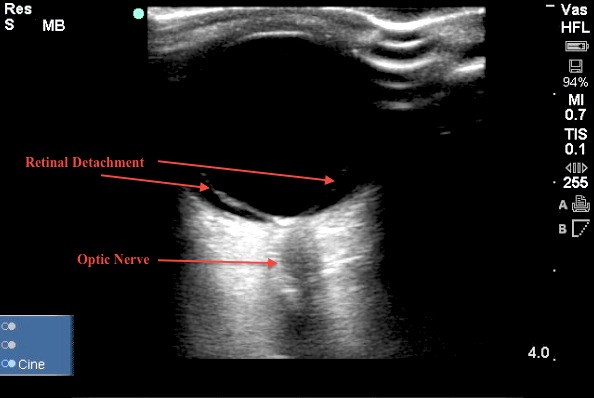
Image 3
Date: April 2013

