We have access to this case because of strong work by Dr. John Diehl, PGY-2, supervised by Dr. Romeo Gallang III, Obstetric Attending. Their patient was a G2P0010 at 11 weeks and 3 days gestational age who presented to OB triage reporting left lower abdominal pain.
Dr. Diehl saw her on her third visit. She clarified to him that she was having LLQ and L upper thigh pain.
On exam:
HR 112, BP 111/72, SpO2 100% on room air
Abdomen: mild tenderness LLQ, moderate tenderness L inguinal fold and upper thigh.
GU: no cervical motion or adnexal tenderness
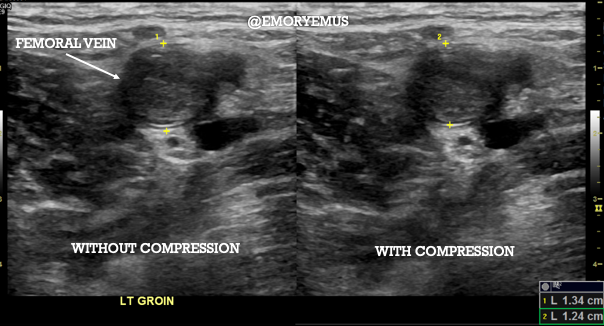
Dr. Diehl performed a focused ultrasound along the left inguinal fold, showing the appearance of the lower extremity deep veins with compression.
He found occlusive thrombus within the common femoral vein:
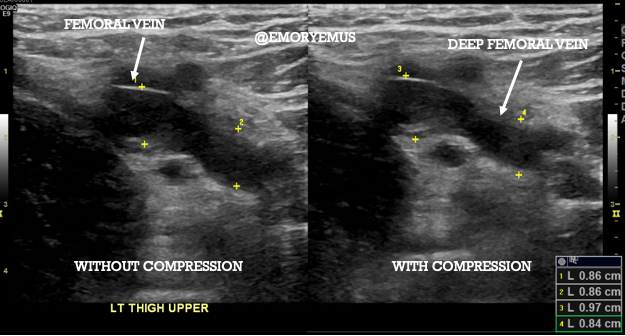
He found occlusive thrombus within the ("superficial") femoral vein and deep femoral vein:
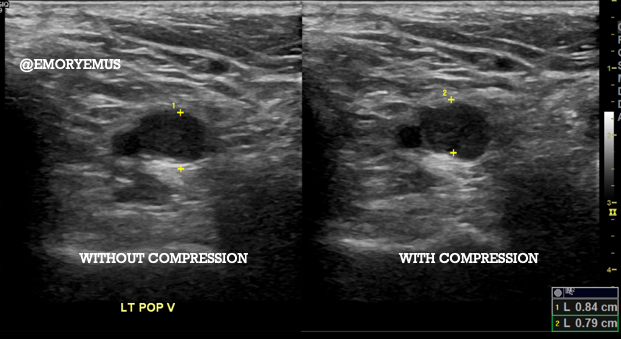
More occlusive thrombus in the popliteal vein:
A normal deep vein exam should demonstrate complete coaptation of the vessel walls, like this:
Or this:
Or this:
Wait. Scroll back up to that last one again. Look closely. Before this vessel compresses, it pulsates. That’s the artery being compressed, the vein does not budge. Depending on the chronicity of the thrombus, it may show various degrees of echogenicity (brightness). Despite the vein looking ‘"empty" it is noncompressible. One way to be certain you’re applying sufficient pressure for vein compression is that the adjacent artery should begin to indent just slightly.
Venous thromboembolism is a leading cause of maternal mortality in the U.S, and DVT risk increases 5-fold during pregnancy. Eighty-two percent of pregnancy-related DVTs occur in the left lower extremity, thought to be due to compression of the left common iliac vein by the right common iliac artery as the uterus enlarges. Ultrasound is often inadequate for the assessment of pelvic (iliac) DVT, so if your clinical suspicion is high and your ultrasound is negative, consider MRI.
Clinical Course:
The patient had no prior history of VTE, but had a second-degree relative with history of unprovoked DVT. She was started on weight based enoxaparin BID. Her work-up was negative for factor V Leiden, prothrombin gene mutation, or antiphospholipid antibody syndrome. Testing for protein C and S deficiency, and antithrombin III deficiency was deferred due to inaccuracy during pregnancy. Because she did not have dyspnea, chest pain, hypoxia, and her tachycardia resolved, no further imaging was pursued to investigate pulmonary embolism. She was recommended to increase her enoxaparin dose as needed as she gained weight throughout pregnancy. She will stop anticoagulation either when contractions begin or 24hrs before a planned delivery. Her post-partum plan is to resume enoxaparin 4-6 hours after vaginal delivery or 6-12 hours after cesarean section and continue until 6 weeks post-partum. She was instructed to avoid estrogen-containing forms of birth control in the future.
Awesome catch Dr. Diehl!
February 18, 2021

