This week's image goes to Dr. Eric Deutch, PGY1, for his ultrasound demonstrating the "lung monster." In the image below, Dr. Deutch found a collection of free fluid. We see fibrinous bands dancing inside a large pleural effusion. His patient had a history of cirrhotic liver disease and hepatic hydrothorax.
Image 1
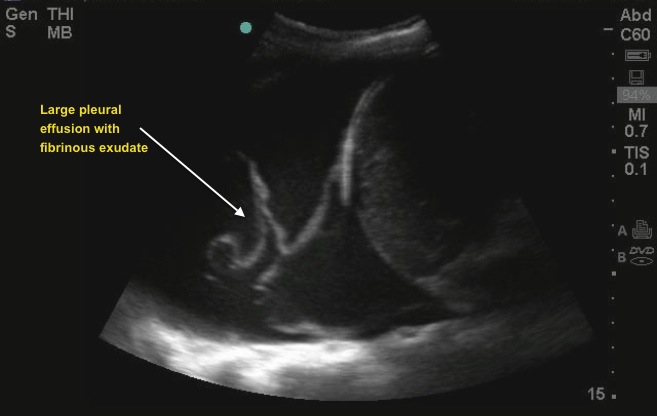
Pleural effusion is an abnormal increase in the volume of pleural fluid. Fluid escapes from the blood vessels and lymphatics of the pleural surface as a result of a pathologic process. Ultrasound is excellent in diagnosing the presence and volume of pleural fluid, and in assessing whether the fluid is amenable to aspiration. Pleural effusions may be characterized as transudates or exudates. Aspiration and chemical analysis of the fluid is needed to differentiate the type of effusion. Both will generally appear anechoic on ultrasound. The fluid that contains floating debris or has septations or fibrous strands is typically an exudate. Ultrasound is exceptionally valuable in localizing pleural fluid and in guiding diagnostic or therapeutic thoracentesis.
To obtain this image, use the curvilinear (abdominal) probe and place it with the indicator marker towards the patient's head on the lateral chest wall (as if you are performing a FAST exam).
Image 2

When present, a layer of anechoic pleural fluid will be seen between the diaphragm and the lung above. The usual mirror image artifact above the diaphragm is absent. Atelectasis is always present with pleural effusion. An abnormal volume of pleural fluid releases the adhesive tension that holds the surface of the lung against the chest wall and the lung reflexly collapses. The atelectatic lung is seen as a wedge-shaped echogenic mass moving with respiration within the pleural fluid. Ultrasonographic signs that indicate that a pleural lesion is fluid that can be aspirated are: (a) change in the shape of the lesion with respiration, (b) floating echodensities, and (c) moving fibrous strands.
July 2013

