Highlights of the MD Curriculum
The MD curriculum was designed by the faculty and student leadership in keeping with the following desired characteristics of Emory School of Medicine graduates.
- Superb clinicians who demonstrate the highest degree of professionalism, outstanding clinical competency and problem-solving skills, and the ability to understand and utilize basic science in the clinical setting
- Curious and creative thinkers with the ability to utilize available resources to answer clinical and research questions and to assess information critically
- Lifelong adult learners with the ability to take ownership of their own present and future educational needs
- Physicians who continue to be passionate about medicine and about making a difference, who are involved in and appreciate efforts to improve the health of local and global communities, and who see medicine as a profession that seeks to address issues of social justice
- Physicians committed to understanding the sociological, psychological, and economic issues of the patient, the family, and the community
- Future leaders eager and able to play leadership roles in their chosen field of medicine or biomedical science, and in their community
Benefits
The Emory University School of Medicine MD curriculum prepares you to:
- Cultivate professional attitudes and behaviors under the guidance of skilled clinicians
- Integrate basic and clinical science
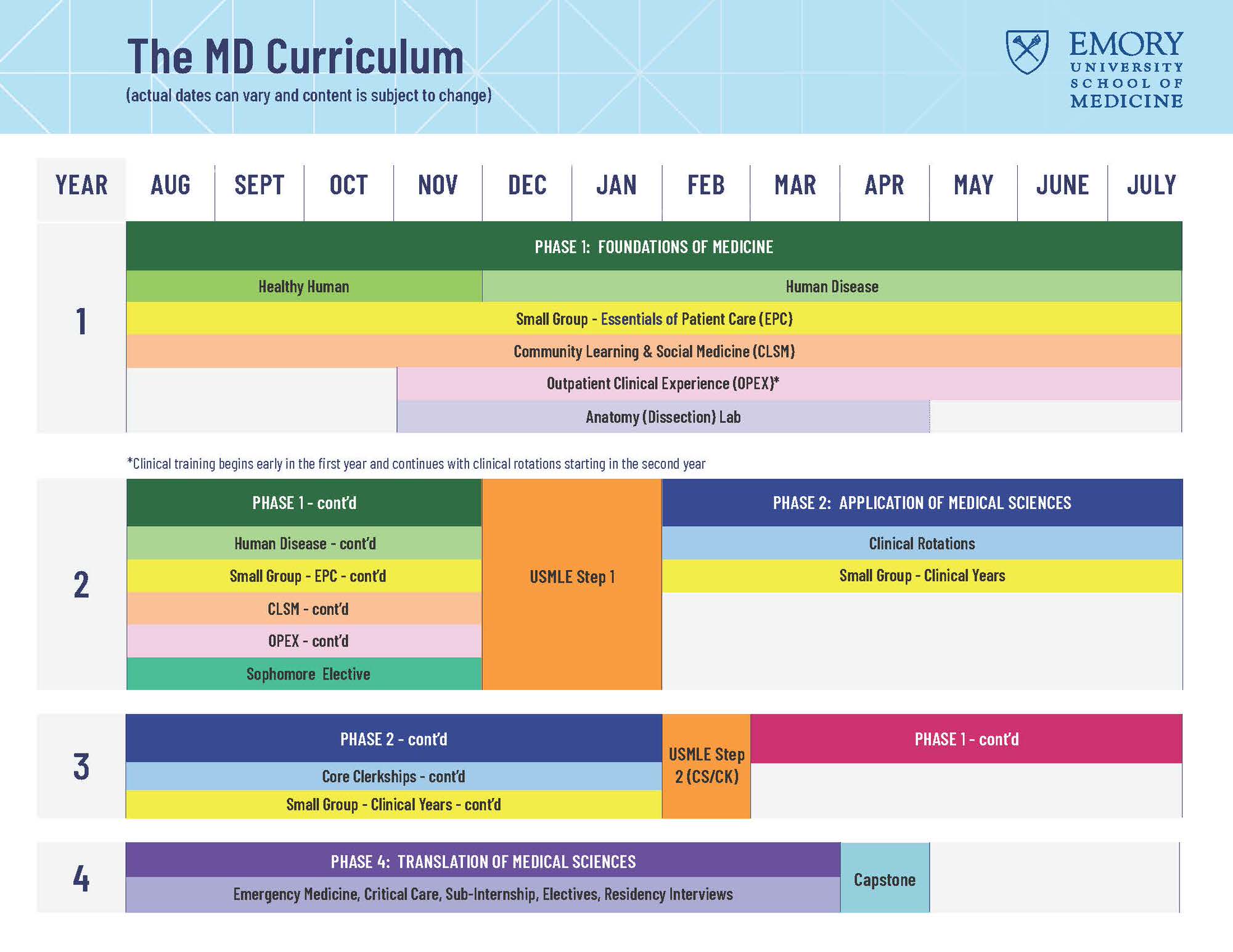
- Begin clinical clerkships in the middle of the M2 Year
- Complete all core rotations before applying to residency programs
- Gain valuable hands-on exposure to specialty and subspecialty fields
- Graduate with the experience of completing their own research project; writing an academic paper; and acquiring presentation skills
- Benefit from a diverse and committed faculty
- Develop close, one-on-one relationships and mentorships with multiple faculty members
- Develop supportive relationships with small group classmates, spanning the entire four years of medical school
- Care for patients earlier
- Understand and meet the needs of our evolving communities and populations
- Develop critical professional attitudes and skills that foster compassion and empathy
- Develop team leadership skills with healthcare professionals from other disciplines, such as physician assistants, nurses, medical imaging specialists, genetic counselors, and physical therapists
- Practice critical skills in simulated, highly realistic team-training exercises
- Graduate well-prepared for life as a successful and fulfilled physician