PFTeach is an online educational tool open to Emory residents, medical students, and the entire Emory medical community. PFTeach was designed to help students feel more comfortable with interpreting PFTs and associated tests, ranging from basic to more subtle findings. This site will be enhanced as we add more PFTs, diagnostic tests (such as X-ray/CT images), CPETs (cardiopulmonary exercise tests), and ventilator waveform analysis. The goal of the site is to help users better understand the interpretation and use of these important non-invasive diagnostic tools.
PFTeach was developed by the Emory Pulmonary and Critical Care fellowship team to improve educational resources within our institution.
We welcome the submission of new content! Submitted cases should be associated with an image (PFTs, x-rays, CT scans, other tracings -- no patient identifiers please!), a question with at least four possible choices, and an explanation for the correct answer. All submissions will be peer-reviewed and, if accepted, posted to the site crediting the author. Email us at pfteach@emory.edu with any submissions or questions.
Select Interaction
Select cases that have all of the following diagnoses:
The correct answer is c)
EIB is the phenomenon of airway narrowing following the onset of physical activity or exercise. It is thought to be triggered when the airways are exposed to a high flow of unconditioned, dehumidified air, allergens and pollutants. Under these conditions there is desiccation of the airway epithelium that in turn leads to a pro-inflammatory cascade. It is common that symptoms are not triggered in warm, moist environments such as pools because the airway desiccation does not occur.
Note that the PFT’s show significant airflow limitation with a decreased FEV/FVC ratio and decreased FEV1 as well as air trapping (increased RV) with preserved DLCO. Also note that there is a significant bronchodilator response (increase in FEV1 or FVC by 200ml and 12%).

2. A 35 year old G2P2 female presents to your clinic progressive fatigue and and shortness of breath with moderate exertion for the past 6 months. She has a 2-pack year history of smoking and is otherwise healthy. She tells you that about the same time her symptoms began she discontinued her oral contraceptives in an effort to have another child. What lab test would help you better interpret diminished DLCO?
The correct answer is c)
The correct answer is C, hemoglobin. Our patient may have developed anemia after discontinuation of her oral contraceptives and resumption of her menstrual cycle. The DLCO measures the ability of gas to transfer from air into the blood. It is measured using a single breath hold of carbon monoxide as it has a high affinity for hemoglobin and readily crosses through the alveolus into the capillaries. Anemia effectively reduces the pulmonary capillary blood volume, which reduces amount of carbon monoxide absorbed. This will in turn cause a reduction in measured DLCO.

3. A 29-year-old woman presents to your office for evaluation of cough. She complains of 3 years of cough accompanied by shortness of breath whenever exerting herself beyond activities of daily living. Her cough is not associated with meals, lying flat or burning epigastric pain. She has no complaints of nasal congestion, seasonal allergies or sinus pressure. Her HEENT exam reveals normal appearing turbinates. Initial spirometry is shown below. At the time of testing she had no respiratory complaints. What is the best next step to confirm the etiology of her cough?
The correct answer is c)
The correct answer is C, methacholine challenge. Chronic cough is defined as a cough that lasts for 8 weeks or longer. The three most common causes are cough variant asthma, upper airway cough syndrome (previously known as post-nasal drip syndrome) and gastroesophageal reflux (GERD). The patient gives a history of symptoms brought on by exertion but has normal PFTs at rest. Since asthma is an episodic disease normal PFTs do not exclude the diagnosis. A provocation test with methacholine may unmask her airflow limitation and aid in your diagnosis.

4. Does the following patient have a significant response to bronchodilator therapy?
The correct answer is b)
The correct answer is B. The ATS defines bronchodilator responsiveness as an improvement of either FEV1 OR FVC by ³12% AND ³200ml. Note that a negative bronchodilator response by ATS criteria should not preclude a trial of bronchodilator therapy if clinically indicated, as patients may still derive symptomatic benefit from their use.

5. Which of the following would likely improve this patient’s PFTs?
The correct answer is b)
This patient’s spirometry is notable for a decreased FEV1 and FVC, but a normal FEV1/FVC ratio. While this is suggestive of restrictive physiology, his TLC and RV are normal, ruling out restriction. Of note, however, the patient does have a significantly decreased MVV, which raises the likelihood of neuromuscular weakness as an etiology. Of the available choices, Mestinon is the only option that would improve an etiology of neuromuscular weakness (in this case, myasthenia gravis).

6. This patient’s condition is most likely to be caused by which of the following?
The correct answer is a)
A decreased FEV1/FVC ratio, decreased FEV1 and elevated TLC and RV indicate airflow limitation (obstruction) with hyperinflation and air trapping. Emphysema and asthma (options a and c) are compatible with this pattern. One would expect DLCO to be normal in asthma and reduced in emphysema, hence option a is correct. Pulmonary arterial hypertension (option b) can be associated an isolated decrease in DLCO and lung fibrosis (option d) would show a restrictive rather than obstructive PFT pattern.

7. Which of the following is most likely to be present in a patient with these PFTs?
The correct answer is b)
This patient’s PFTs are compatible with a restrictive process, as evidenced by a normal FEV1/FVC ratio, and decreased FEV1, FVC, TLC, and DLCO, most likely fibrosis. In fibrosis, loss of normal lung architecture leads to “pulling” of the airways, which manifest as traction bronchiectasis (option b). Emphysema and asthma are characterized by a loss of elastic recoil (option a) and reversible airway bronchoconstriction (option c) respectively. At the same time, these conditions would show an obstructive PFT pattern. Lastly, mediastinal lymphadenopathy by itself should have no effect on PFTs. This can be seen in stage 1 sarcoidosis.

8. Pt is a 24 y/o F with a history of bilateral lung transplant for cystic fibrosis 3 years ago. She presents to clinic with worsening shortness of breath. What is the likely cause of her shortness of breath?
The correct answer is d)
The PFTs show moderately severe airflow limitation without any bronchodilator response. ILD is incorrect because these PFTs do not show a restrictive pattern. COPD is unlikely based on her age. Her flow volumes are not consistent with a fixed airway obstruction, making airway stenosis unlikely. In any patient with shortness of breath after a lung transplant, the concern is for chronic rejection, which is manifested by bronchiolitis obliterans. It is a fibrotic process resulting in progressive narrowing of bronchiolar lumens and airflow obstruction is noted on PFTs.

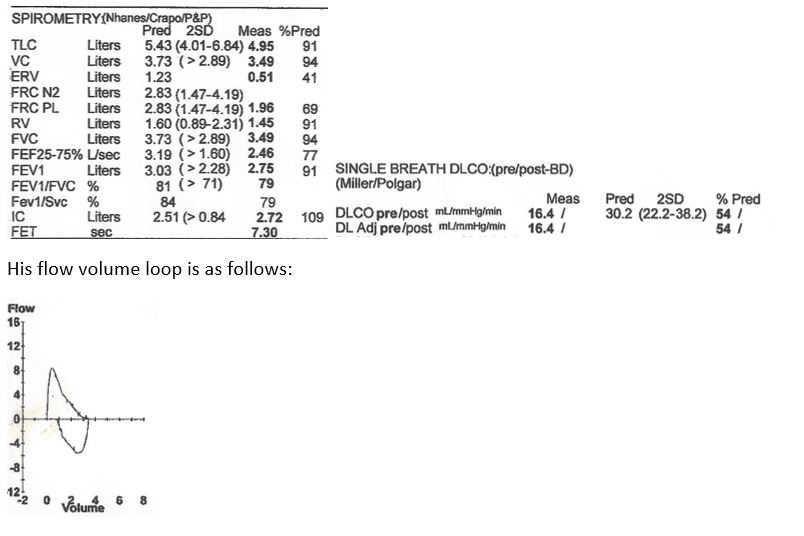
9. Pt is a 55 y/o M with a history of tobacco abuse who presents to clinic for evaluation of progressive shortness of breath. Which of the following interventions is likely to prolong his lifespan?
The correct answer is e)
Pt’s spirometry and flow volume loop are consistent with moderately severe airflow limitation. He also has evidence of airtrapping with an elevated RV with a low DLCO. Thus, he likely has emphysema.
In the setting of a DLCO less than 40% predicted, hypoxia is highly likely. The only measure shown to improve survival in emphysema has been the use of oxygen in patients who have evidence of hypoxia.

10. A 64 y/o M presents to clinic with progressive shortness of breath, fatigue, and dry cough over the past year. He denies weight gain, chest pain, fevers, and lower extremity edema. Which of the following would you expect to find in this patient?
The correct answer is c)
This patient’s PFTs show a restrictive pattern with a very low DLCO. This in combination is indicative of interstitial lung disease. Choice A is seen in HHT, which commonly presents as pulmonary vascular disease in the pulmonary clinic. B and E are seen in COPD and asthma respectively. Choice D is seen in aortic regurgitation. Traction bronchiectasis is a common finding in CTs of patients with ILD.

11. Pt is a 32 y/o F who presents to lung transplant clinic for evaluation for possible transplant. She has been sick since infancy and has had issues with chronic cough, copious sputum production, shortness of breath, and repeated lung infections. She has never smoked and has no family history of lung disease. Based on her PFTs and clinical history, which of the following is her underlying disease process?
The correct answer is a)
This patient’s spirometry and flow volume loop reflect a very severe airflow limitation with a low DLCO as well as airtrapping. IPF and NSIP both have restrictive patterns so are not the correct answers. Although this PFT pattern can be seen in COPD, the patient’s age and lack of smoking make it highly unlikely for this to be COPD. Asthma should not cause a low DLCO.

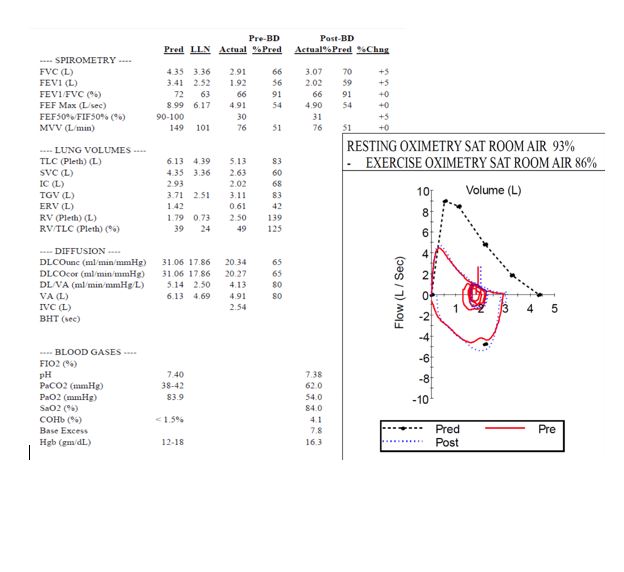
12. You are asked to perform a preoperative assessment for a 64 year-old female who has stage IA adenocarcinoma in the left upper lobe of her lung. She has smoked 1 pack of cigarettes per day for 40 years, has non-insulin dependent diabetes mellitus and has had no prior surgeries. She becomes very dyspneic with walking one flight of stairs but otherwise has no dyspnea at rest. In your office she is afebrile, her blood pressure is 119/69 mmHg, heart rate is 83 bpm, SpO2 on room air is 93% and body-mass index is 24 kg/m2.
Assuming that the planned surgery is a left upper lobectomy, what is her predicted postoperative FEV1?
The correct answer is d)
The equation for predicting postoperative FEV1 is: preoperative FEV1x(1-(segments to be removed/18)). This is important since a predicted postoperative FEV1 <40% predicted is a marker for increased risk of morbidity and mortality from lobectomy and may be an indication for further testing before surgery or that the patient is not a candidate for lung resection.
Note that the PFT’s are typical of a patient with emphysema. The flow-volume curve reveals severe airflow limitation, spirometry reveals an obstructive defect (decreased FEV1/FVC ratio and FEV1), and lung volume analysis reveals hyperinflation and air-trapping (increased TLC and RV, respectively).
Brunelli et al. Physiologic Evaluation of the Patient With Lung Cancer Being Considered for Resectional Surgery. CHEST 2013; 143(5)(Suppl):e166S–e190S
In this case:
4 segments are being removed (LUL including lingula); thus 0.73 L x (18-4/18)= 0.57 L

13. A patient with longstanding chronic obstructive pulmonary disease returns to your clinic with the following pulmonary function tests. Based on these tests, which therapy would you recommend?
The correct answer is b)
This patient has moderate stage obstructive lung disease. This is evidenced by a low FEV1, FVC and FEV1/FVC ratio with additional evidence of air trapping from the increased RV. The bronchodilator challenge does not show a 200ml or 12% increase in either the FEV1 or FVC. While the GOLD guidelines recommend bronchodilator therapy at the moderate stage of COPD, it does not recommend inhaled steroids until the very severe stages of COPD (FEV1 < 0.50) and with frequent exacerbations. The patient has further evidence of a compensated respiratory acidosis with hypercarbia but low normal pH. Finally, the exercise oximetry shows a that SpO2 is < 88% with exertion qualifying the patient for oxygen therapy with exertion. While bilevel positive airway pressure ventilation is being studied in advanced obstructive lung disease, results are not consistent.
Of note, there is a discrepancy between pulse oximetry and oxygen saturation on the ABG. This is explained by the elevated presence of Carboxyhemoglobin (normal < 1.5%), which is interpreted as oxyhemoglobin by the pulse ox, but differentiated on co-oximetry. Elevated CO is frequently seen in active smokers.
14. You see a patient in your office for dyspnea. She is a 55 year-old woman with no other past medical history other than asthma as a child that resolved in her teenage years. She has never smoked tobacco. She has been experiencing mild to moderate dyspnea nearly daily for several years, sometimes at rest and exacerbated with walking more than approximately 100 feet on flat ground. She has no cough or wheezing and there is no seasonal variation in her symptoms.
Her vital signs are as follows: blood pressure 161/80 mmHg, pulse 93 bpm, oral temperature 37.3 °C (99.1 °F), SpO2 94%.
What is the most likely reason for her abnormal arterial blood gas?
The correct answer is e)
The clinical presentation and pulmonary function test are most consistent with obesity hypoventilation syndrome. On spirometry we see that she has a reduced FEV1 and FVC but a preserved FEV1/FVC ratio. With a normal TLC, this could represent mild airflow limitation from obstructive lung disease or restrictive disease. The other clues here are that she has a low ERV (expiratory reserve volume). This is the air left in the lungs at end of a maximal exhalation and can be reduced in the morbidly obese or in patients with large volume ascites given the body habitus pushing upwards on the diaphragm and thoracic cavity. This compression of the thoracic cavity explains the restrictive pattern seen on spirometry. This degree of obesity has also led to obesity hypoventilation syndrome with a mild, compensated respiratory acidosis and mild hypoxemia.

15. You are asked to evaluate a patient with dyspnea. The patient is a 57 year-old man with progressive dyspnea on exertion over the prior two years. He now can only walk 50-100 feet before having to stop to catch his breath. He has a mild, daily dry cough. He has smoked 1.5 packs of cigarettes daily for 30 years and is trying to cut down but has not been able to quit. He has worked as a cook for over 20 years, has no pets at home, no water damage in his house.
His vital signs are as follows: blood pressure 165/92 mmHg, pulse 104 bpm, oral temperature 35.8 °C (96.4 °F) SpO2 93%. His exam reveals no wheezes or rhonchi but some diffusely diminished air entry.
What is the next best recommendation?
The correct answer is c)
This patient has severe airflow limitation secondary to obstructive lung disease evidence by a low FEV1 and FVC with a low FEV1/FVC ratio. There is additional evidence of air trapping with a very high RV (residual volume). Furthermore, the spirometry exhibits a positive bronchodilator response defined by a greater than 12% and/or 200mL increase in either the FEV1 or FVC. This patient has improvement in both FEV1 and FVC, therefore, the first initial step in treatment is to start bronchodilator therapy. His exercise oximetry does not reveal a SpO2 < 88% to qualify him for benefits from long-term oxygen therapy. While bilevel positive airway pressure ventilation is being studied in advanced obstructive lung disease, results are not consistent. Given his robust bronchodilator response this should be the initial therapy of choice.

16. A 46 year-old female is referred to you for evaluation of dyspnea and abnormal pulmonary function tests. She has been experiencing shortness of breath over 1-2 years, progressing to where she is now dyspneic with two flights of stairs. During this time she has had a dry cough and an unintentional 20 pound weight loss but no fevers, chills or night sweats. She has no leg swelling, orthopnea or chest pain. She smoked 1 pack per day for 20 years but quit 10 years ago. She works as a receptionist and has no pets at home, travel or water damage in her house. She had an uncle who died of sarcoidosis.
In your office she is thin but otherwise healthy appearing. Her vital signs are as follows: blood pressure 113/83 mmHg, pulse 115 bpm, oral temperature 36.4 °C, room air SpO2 94% and BMI 19.5 kg/m2. She has diffuse, bilateral rales and the rest of the physical exam is normal.
Which of the following statements is most accurate regarding her pulmonary function tests?
The correct answer is c)
This patient has pulmonary sarcoidosis with extensive parenchymal fibrosis. Her pulmonary function tests show a restrictive defect characterized by a reduction in FEV1 and FVC with a preserved FEV1/FVC ratio and a reduction in TLC. Furthermore, her DLCO is low, indicating an impairment in oxygen transfer secondary to fibrotic lung disease.

17. A 55 year-old female comes to your clinic and you are given a copy of her PFTs as shown. Which of the following physical examination findings is most likely to be found?
The correct answer is b)
This patient’s PFTs show restrictive disease with a TLC of 49% percent predicted and a low DLCO of 27% suggesting underlying ILD. Of the above physical examination findings, fine inspiratory crackles would be most likely heard in a patient with ILD.

18. A 45 yo F presents to your clinic with a chronic cough. She reports that the cough is dry and present throughout the day but wakes her up several times at night. She is tired of being unable to sleep at night and wants to know what to do next. Based on her PFTs you decide to:
The correct answer is c)
Though she has normal PFTS a night time cough could still be symptoms of asthma and would warrant treatment. Patients with asthma can have normal PFTs. Sending her for a methacholine chachallenge test, if negative might help rule out asthma as a cause of her chronic cough.
19. A 28 year old male with a history of peanut allergy and eczema as a child comes to see you in clinic for worsening shortness of breath. He reports that he has a night time cough associated with a runny nose that cause him to wake up at night feeling short of breath. He also notes that when he goes on his runs he now has to stop and catch his breath at the top of a hill. He sometimes notices that his breathing may be noisy. His younger brother also has asthma. He performs a methacholine challenge test and his results are shown below. Based on this test you decided to:
The correct answer is b)
The methacholine challenge test is markedly positive as the patient has a drop ≥ 20% of his FEV1 with less than 1mg/mL of methacholine (note our patient’s PC20 is at 0.160mg/mL of methacholine). This in and of itself is not diagnostic of asthma, but based on his positive test and clinical symptoms asthma is the most likely diagnosis and warrants treatment.

20. A 42 year old female comes to your clinic after being hospitalized for a reported asthma exacerbation. She received several breathing treatments with nebulizers and a course of steroids. Despite this she continues to be short of breath and not getting better. You get her spirometry as shown below and decide the next best step would be:
The correct answer is c)
Though her spirometry shows no evidence of air flow limitation, her flow-volume loop shows flattening of her inspiratory loop which is concerning for extrathoracic obstruction such as vocal cord dysfunction. This also doesn’t improve with steroids.

21. The etiology of this person's lung pathology is most likely:
The correct answer is b)
This pft is most consistent with COPD, given its low FEV1/FVC and its low DLCO. Connective tissue disease most commonly causes restrictive lung disease. PE will cause a drop in DLCO with normal FEV1 and FVC. Atopy is most commonly associated with asthma. While this PFT shows obstruction, the low DLCO is atypical in asthma.

22. This patients FRC is most likely:
The correct answer is a)
This patients pfts show a significant obstruction(likely COPD). Furthermore, the Residual Volume (RV) is quite elevated. This suggests air trapping due to the inability to fully exhale prior to taking the next breath. Thus, the baseline respiratory volume is elevated, and FRC must be elevated.

23. This patient has evidence of airflow limitation, and underwent a bronchodilator challenge. Do they show evidence of reversibility?
The correct answer is b)
A positive bronchodilator response is defined as an increase in FEV1 of 12% AND 200 cc.

24. This pft is consistent with which of the following diseases?
The correct answer is c)
The low TLC and and DLCO are consistent with a restrictive disease-such as interstitial lung disease (eg IPF).

25. If measured, the TLC in this patient would most likely be:
The correct answer is c)
These results are most consistent with a restrictive defect-the FEV1 and FVC are both very low, and the FEV1/FVC is normal. Thus, the TLC would likely be low, as seen in restrictive disease.

26. A 36 year-old male smoker presents to your office for evaluation of long-standing uncontrolled asthma. Patient was admitted five times to the ICU, requiring mechanical ventilation each time. Most recently was one month ago when he was intubated, weaned, and liberated within 24 hours. His flow-volume loop is seen below. What diagnosis should you be considering?
The correct answer is c)
The flow-volume loop shows a variable extrathoracic obstruction pattern where the inspiratory loop is blunted with an overall spared expiratory loop. This can be seen classically in VCD, a disease where the vocal cords paradoxically close during inspiration. This can be diagnosed by laryngoscopy with visualization of the vocal cords during tidal breathing. Treatment for this condition often requires vocal cord retraining exercises.

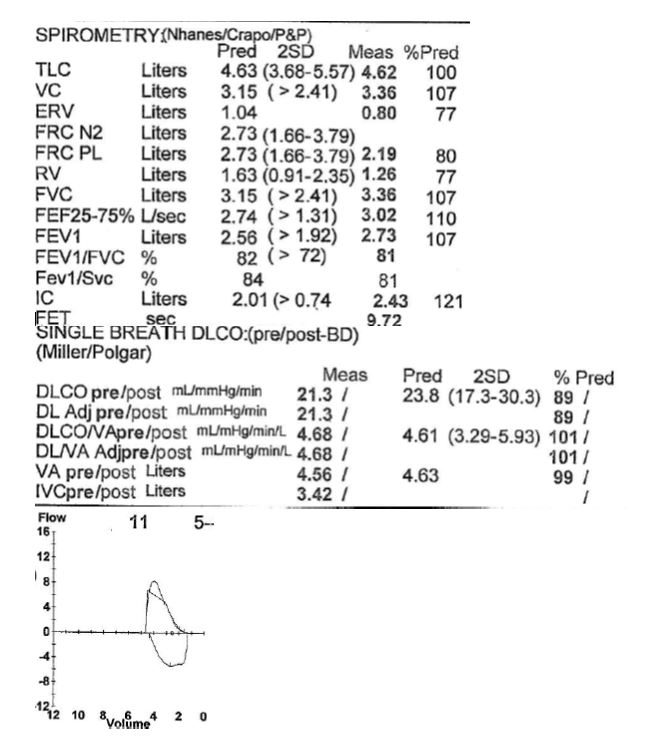
27. Which of the following best describes the pulmonary function test seen below?
The correct answer is b)
Restrictive pattern with volume loss. The above PFT shows a FEV1/FVC which is within 2 standard deviations of the predicted FEV1/FVC. The FEV1 and FVC are both below the lower-limit-of normal (defined as 2 standard deviations from the predicted). The TLC and RV are both decreased. Airflow limitation (obstructive pattern) would have a decreased FEV1/FVC. A mixed pattern would have both a decreased FEV1/FVC and a reduced TLC, suggestive both airflow limitation AND volume loss. To further characterize this restrictive pattern, the next step would be to assess DLCO to determine if this is due to interstitial lung disease OR chest wall/neuromuscular problems.

28. What kind of abnormality is seen in this flow-volume loop?
The correct answer is d)
The above flow-volume suggests a fixed obstruction. Both the inspiratory loop and expiratory loop are blunted suggesting overall decrease in upper airway caliber during the entire respiratory cycle. Other things that can cause this are upper airway tumors (i.e. tracheal masses) or large goiter that is obstructing upper airway. COPD would result in a characteristic “scooping” in the expiratory limb. Vocal cord dysfunction would typically show a variable extrathoracic defect, with blunting of the inspiratory loop. (Remember, vocal cords are normally open during inspiration, but in VCD they tend to close.) Lastly, IPF would show a restrictive pattern on flow-volume loop (ie tall, skinny loop with volume loss).

29. Patient is a 60 year old male who presents to your clinic for abnormal chest imaging. Three weeks ago, he presented to emergency room with some slight hemoptysis. There, a chest xray was concerning for a right sided lung mass. He is here for further evaluation. On history, patient is complaining of 6 months of dyspnea on exertion, cough with occasional sputum production, and 30 lb weight loss. PFTs above are most consistent with what diagnosis?
The correct answer is b)
The above PFTs show an airflow limitation. The FEV1/FVC ratio is decreased at 46% of the predicted. Both the FEV1 and FVC are both reduced. No lung volumes were not done. Also, the flow-volume loop show characteristic “scooping” in expiratory loop. This is characteristic of obstructed diseases such as COPD and asthma. IPF, obesity, and hypersensitivity pneumonitis usually show a restrictive pattern on PFTs, where you have decreased FEV1 and FVC but the FEV1 and FVC would be normal or supranormal. Confirmation would then be made by determining lung volumes. According to the question stem, the patient also has a history of lung cancer, likely from smoking. This, along with airflow limitation as above, suggests emphysema.

30. The pulmonary function tests shown below were obtained from a 26 year old Caucasian male smoker who was being seen for intermittent dyspnea. His BMI is 40 kg/m2.
Which of the following statements are correct?
The correct answer is a)
BMI has been shown to have a significant effect on lung volumes. FRC and ERV (option A) have been shown to decrease approximately 3% and 5%, respectively, for each unit increase in BMI from 20 to 30 kg/m2.1 Smaller decreases are seen in TLC, VC and RV. Spirometry results can be normal in asthma patients who are not having an exacerbation (option B is incorrect). A significant bronchodilator response is defined as an ≥12% and 200ml increase in FEV1 or FVC above baseline after the administration of a bronchodilator (option C is incorrect).
References
1. Jones RL, Nzekwu MM. The effects of body mass index on lung volumes. Chest 2006;130:827-33.

31. You are reviewing the pulmonary function tests of a 50 year old Hispanic male who has a 20 pack year smoking history and a BMI of 43 kg/m2. He is being evaluated for dyspnea on exertion. The results of his spirometry are shown below.
RV, TLC and DLCO are normal.
Which of the following is the correct interpretation of his spirometry results?
The correct answer is d)
This patient has a non-specific spirometric pattern which is defined by having a reduced FVC and/or FEV1, a normal FEV1/FVC ratio and normal lung volumes. A longitudinal study of 1284 patients with an initial non-specific pattern showed that 64% of patient continued to show this pattern on follow up with only 15% progressing to an obstructive pattern and a further 16% progressing to a restrictive pattern.1 A normal FEV1/FVC ratio excludes airflow limitation (options A and B are incorrecct) and lung volumes are normal (option C is incorrect).
References
1. Iyer VN, Schroeder DR, Parker KO, Hyatt RE, Scanlon PD. The nonspecific pulmonary function test: longitudinal follow-up and outcomes. Chest 2011;139:878-86.

32. A 51 year African-American male with chronic exertional dyspnea is referred for PFTs by his primary care physician. You note that he has 20 pack-year smoking history and has a BMI of 41 kg/m2. The results of his study are shown below.
The results are most consistent with which of the following diagnoses?
The correct answer is b)
This patient has restriction which is suggested by decrease in his FEV1 and FVC with a normal FEV1/FVC ratio and is confirmed by his low TLC. He also has a decreased diffusion capacity. The flow-volume loop is narrow with a tall expiratory limb. This findings are most consistent with a diagnosis of stage IV sarcoidosis (option B). Morbid obesity can cause a restrictive pattern but does not explain the reduction in DLCO (option D is incorrect). Restriction is not a feature of asthma, emphysema or primary pulmonary hypertension (options A, C and E are incorrect).

33. The flow volume loop below is most consistent with which of the following patterns?
The correct answer is b)
The flow-volume loop shown above is small, with a “scooped out” appearance of the expiratory limb. There are reduced flow rates at all lung volumes. There is only a marginal increase in post-bronchodilator flow rates. This pattern is seen with airflow limitation (option B is correct). Patients with restriction have narrow flow-volume loops with tall steep expiratory limbs (option A is incorrect). The flow-volume loops seen in variable extrathoracic and intrathoracic obstruction have flattened inspiratory and expiratory limbs respectively (options C and D are incorrect).

34. You are evaluating a 56 year old female with severe dyspnea on exertion. The results of her PFTs are shown below.
Based on her PFTs, which of the following would be the most likely finding on her chest X-ray?
The correct answer is c)
This patient has severe airflow limitation, air trapping and a decreased DLCO. These findings are commonly seen in patients with emphysema who can present with features of hyperinflation on chest xray including increased retrosternal air space.

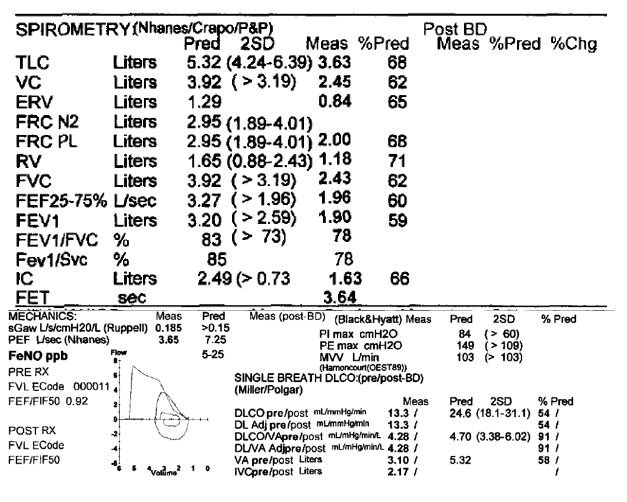
35. 71y/o male with a history of asthma, diagnosed as a child, presents with worsening shortness of breath not controlled on bronchodilators and persistent dry cough. Which of the following statements is true?
The correct answer is c)
Based on his PFTs, patient has a mixed defect. Spirometry shows evidence of severe airflow limitation (FVC <70% and FEV1 35-49%). Additionally, decreased lung volumes (TLC <LLN) suggestive of superimposed restrictive defect. This is likely due to asthma causing the obstruction and recent diagnosis of cryptogenic organizing pneumonia producing the restrictive pattern.

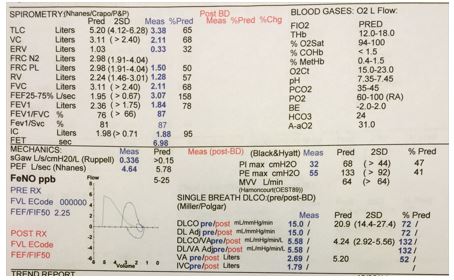
36. 68y/o male with a history of obesity, sleep apnea and 45 pack year smoking history presents for evaluation for worsening shortness of breath over the past 3-4 years. No evidence of crackles on lung auscultation. CXR obtained during a recent ER visit does not show any abnormalities. Which of the following statements is true?
The correct answer is e)
Based on his PFTs, patient has evidence of a mixed defect. Spirometry shows evidence of moderately severe airflow limitation with a significant bronchodilator response that can be attributed to his significant smoking history. Additionally, lung volumes show evidence of moderate restrictive defect. In the setting of normal CXR and lung auscultation, patient’s restrictive defect can be attributed to his body habitus. Patient will benefit from bronchodilators for his COPD and diet/exercise to lose weight.

37. 19y/o female with a history of progressive lower extremity weakness and neuropathy over the past few years presents with SOB and cough with exertion. What is the most likely cause of her PFTs?
The correct answer is b)
This patient’s PFTs show evidence of significantly reduced maximum inspiratory pressure (PI max) and maximum expiratory pressure (PE max) which in the setting of her progressive weakness and neuropathy likely reflects involvement of inspiratory and expiratory muscles, and diaphragm.

The correct answer is b)
The PFT’s are most consistent with interstitial lung disease (ILD). A normal FEV1/FVC ratio with low TLC and DLCO are hallmarks. Spirometry shows no evidence of obstruction. Physical examination findings of ILD often include fine inspiratory crackles.
While morbid obesity can lead to a decreased TLC, it typically does not cause a decrease in DLCO.

39. The PFT’s shown below are most consistent with which diagnosis?
The correct answer is a)
The PFT’s show an isolated low DLCO, which would be most consistent with a diagnosis of pulmonary hypertension. Emphysema and cystic fibrosis should show obstruction, while idiopathic pulmonary fibrosis should show restriction. Asthma may show obstruction at time of testing, or PFT’s may be normal if the patient’s symptoms are under control.

40. Which clinical scenario would be most consistent with the PFT shown below?
The correct answer is b)
The PFT’s are most consistent with a combined obstructive and restrictive defect. The flow-volume curve demonstrates airflow limitation, and the FEV1/FVC ratio, indicative of an obstructive defect. Note the DLCO is also reduced. The TLC is also reduced, indicative of a restrictive process. The clinical scenario above that best describes a combined obstructive and restrictive defect is b.

41. Which combination of physical examination findings would you expect to find in a patient with the following PFT?
The correct answer is a)
The PFT’s are most consistent with severe airflow limitation with hyperinflation, air trapping, and over distention. This is most commonly seen in emphysema, although the DLCO is not shown in this example. The flow-volume curve shows severe airflow limitation. A reduced FEV1/FVC ratio, a severely decreased FEV1, and an increased TLC and RV are hallmarks of emphysema. Physical examination would show a prolonged expiratory phase and hyperresonance to percussion.

42. Which diagnosis is suggested by the PFT seen below?
The correct answer is e)
The PFT reveals (1) severe airflow limitation without a significant bronchodilator response, (2) hyperinflation, air trapping, and over distention, and (3) a severely decreased DLCO. The flow-volume curve shows severe airflow limitation. A reduced FEV1/FVC ratio, a severely decreased FEV1, an increased TLC, RV, and FRC, and a severely decreased DLCO are hallmarks of advanced emphysema.
Note the ABG reveals a chronic respiratory acidosis with appropriate metabolic compensation and hypoxemia.

43. Which of the following conditions would be most likely with the spirometry and additional data below?
The correct answer is a)
The flow-volume loop shows a “scooped” expiratory limb consistent with flow-limitation or obstruction, as could be seen in either asthma or COPD. Similarly, the spirometry shows a reduced FEV1/FVC ratio which could also be seen in either asthma or COPD. However, the patient has an elevated fraction of exhaled NO (FeNO) which is associated with eosinophilic airway inflammation. FeNO has been proposed as a non-invasive biomarker to help guide diagnosis and management of asthmatics. Incidentally, this patient also has a reduced FEV1 and FVC which could be consistent with restrictive lung disease and low lung volumes, but lung volume measurements would be necessary to confirm that diagnosis.

44. This patient is a 65 year-old woman referred to your office for evaluation of shortness of breath. Her pulmonary exam is unremarkable. Based on her pulmonary function tests, which of the following would you recommend?
The correct answer is d)
The correct answer is (d). These PFT's are normal, thus suggesting that the lungs are not the reason for dyspnea. Other organ systems should be considered as the etiology of dysnea.

45. This patient is a 58 year-old woman seen in clinic for progressive dyspnea on exertion. She reports that she is unable to climb a flight of stairs without stopping. Based on her pulmonary function tests, which of the following would you recommend?
The correct answer is a)
This patient has mild restriction on her pulmonary function tests with a total lung capacity that is 79% of predicted. Her flow-volume loop is also consistent with mild restriction and shows a tall, thin expiratory loop that is reflective of increased elastic recoil of the lung. She also has a reduced DLCO which can be seen in a variety of pulmonary diseases, including interstitial lung diseases with pulmonary fibrosis.
A high-resolution CT scan would help characterize the pattern of parenchymal involvement and guide further work-up such as serologies or lung biopsy.

46. Based on the flow-volume loop and spirometry data below, what would you expect to see if this patient had complete lung volume measurements done?
The correct answer is a)
This patient has severe airflow limitation as could be seen with emphysema. Patients with emphysema have decreased elastic recoil of the lungs as a result of parenchymal damage. As a result, an increase in the residual volume is one of the earliest changes that can be seen in COPD on pulmonary function tests. With increasing severity of emphysema the total lung capacity will also increase (corresponding to increasing lung volumes, “barrel chest,” on physical exam).

47. Which of the following is the best explanation for the pulmonary function test results shown below?
The correct answer is c)
COPD is highly unlikely in the absence of airflow limitation (FEV1/FVC ratio is normal, answer A is incorrect). Pulmonary hypertension could present with an abnormal diffusing capacity, as in this case, but would not present with concomitant restriction (TLC is low, answer B in incorrect). Restrictive physiology could be due to either neuromuscular disease or interstitial lung disease; in general, the DL/VA is reduced (or normal) in interstitial diseases and normal-to-elevated in extrapulmonary diseases (chest wall and neuromuscular problems). The low DL/VA suggests interstitial disease, making sarcoidosis the best answer (C is correct).

The correct answer is c)
Patients with chronic obstructive pulmonary disease will show airflow limitation on pulmonary function testing, with both a low FEV1 and a low FEV1/FVC ratio. It is common for them to have a low vital capacity also, but this is generally due to air trapping with an increased residual volume (choice D is incorrect). There is nothing about the flow volume loop that is inconsistent with COPD as a diagnosis (E is incorrect). While a bronchodilator response is more classic for asthma than emphysema or chronic bronchitis, many patients with traditional COPD will have a response to albuterol administration (Tashkin et al, ERJ 2008), making choice A incorrect. A low diffusing capacity that at least partially "corrects" after adjusting for alveolar ventilation is also typical (B is incorrect). Most patients with pure COPD will have a normal-to-elevated total lung capacity. A decreased TLC suggests the presence of an alternative (or concomitant secondary) diagnosis.

49. The most likely cause of this patient’s lung disease is:
The correct answer is a)
There is no evidence of airflow limitation. The patients FEV1 and FVC are reduced suggestive of a restrictive disease and in addition the TLC is severely reduced. The low DLCO and flow volume loop pattern are also consistent with a restrictive pattern all of which can be seen in interstitial lung disease likely secondary to her rheumatoid arthritis.

50. Which of these physical exam findings is most likely present in a patient with the flow volume loop seen below.
The correct answer is b)
• Hyperresonance is a lower pitched sound which occurs in the chest as a result of overinflation of the lung and is usually seen in emphysema or pneumothorax. This patients flow volume loop suggests air trapping, despite a normal FEV1/FVC ratio.
• Egophony occurs in compressed lung from pleural effusion and consolidated lung that connected to a bronchus
• Whispered Pectoriloquy Normal lung filters out low frequency speech, but solid tissue does not. This is very sensitive for a consolidation.
• Crackles are caused by terminal small airway opening affected by interstitial fluid or thickening

51. Which of the following is least likely to present with findings listed above?
The correct answer is c)
Patients with bronchiectasis have a pattern consistent with obstruction which is not seen above (FEV1/FVC >70%). The other 4 choices typically present with a restrictive process with a reduced DLCO.
52. Which of the following conditions can give rise to this PFT result?
The correct answer is a)
PFT shows normal FEV1/FVC ratio (no airflow limitation), reduced TLC (restriction), normal DLCO, and reduced both maximal inspiratory (MIP) and expiratory pressure (MEP). This PFT can be seen in neuromuscular weakness (choice A, correct answer). IPF (choice B) although it could explain a drop in TLC, it should have a decreased DLCO and it could not explain the decrease in MIP and MEP. Pregnancy (choice C) can have a decrease in TLC, ERV, RV, and FRC. But it should not cause a decrease MIP and MEP. DLCO can increase in the first trimester followed by a slight decrease later in pregnancy due to alteration in pulmonary vascular volume. CHF (choice D) can cause decrease TLC. It can also cause airflow limitation and air trapping (increase RV) especially in acute pulmonary edema. DLCO is reduced and can be irreversible in long standing CHF. However, CHF could not explain a decrease in MIP and MEP. Lastly, there is no airflow limitation here thus emphysema (choice E) is not the correct answer.
53. Which is true regarding the PFT of this 55 year-old non-smoker male with history of atopy who presents with episodic wheezing after moving to Atlanta?
The correct answer is a)
This PFT is consistent with airflow limitation with significant bronchodilator response (at least 12% AND 200ml increase of either FVC or FEV1). Thus choice D is incorrect. This PFT along with patient history of atopy and possible allergen exposure in Atlanta make asthma more likely. Choice A is correct. DLCO may be increased in asthma patient. Possible mechanisms are 1) Increase perfusion of the apices of the lung due to increase negative pleural pressure (especially during exacerbation) 2) Overestimation of DLCO due to airflow limitation thus more CO is trapped in the lung. Choice B is incorrect as RV should increase in the setting of air trapping. Choice C is incorrect as this PFT show airflow limitation already, methacholine challenge test will not add any further diagnostic value. Choice E is also incorrect as there is no flattening of the inspiratory limb of the spirometry to suggest variable extrathoracic central airway obstruction.

54. In this 57 year old male with a 40 pack-year smoking history and chronic dyspnea, what likely explains this PFT abnormality?
The correct answer is c)
PFT shows no airflow limitation (choice A is incorrect) but also shows flattening of the inspiratory limb of the spirometry concerning for variable extrathoracic central airway obstruction (choice C which is one of the causes of extrathoracic airway obstruction is correct). Choice B and D (incorrect) causes variable intrathoracic airway obstruction which causes flattening of the expiratory limb of the spirometry. Choice E, pulmonary arterial hypertension could not explain the flattening of the inspiratory limb of this spirometry, therefore, is incorrect.

55. An 80 year old female with worsening dyspnea presents with the PFT shown below. Which of the following medications is the most likely to cause her PFT findings?
The correct answer is e)
The PFT shows no airflow limitation, reduced TLC, and reduced DLCO concerning for pulmonary fibrosis. Amiodoarone can cause pulmonary fibrosis while there is no evidence that the other medications are associated with this condition.

56. Which EKG finding is most common in the patient with this PFT?
The correct answer is a)
The PFT shows severe airflow limitation without significant bronchodilator response along with moderately reduced DLCO consistent with emphysema. Lung hyperexpansion causes flattening of the diaphragm and external compression of the heart resulting in elongation and vertical orientation of the heart (EKG: vertical or right axis deviation). Due to its fixed attachments to the great vessels the right ventricle moves anteriorly and the left ventricle moves posteriorly (Clockwise rotation, choice A). Increased air between the heart and electrodes leads to reduced QRS voltage (choice B). Chronic hypoxemia that causes hypoxic pulmonary vasoconstriction along with reduced pulmonary vascular bed due to destruction of lung tissues with loss of pulmonary capillaries lead to pulmonary hypertension. This can cause RVH, RAE (p pulmonale, choice C), and RBBB. Chronic pressure overload to the right atrium can cause MAT (choice E). MAT increases mortality in patient with COPD. LBBB (Choice D), is not a common findings in patient with emphysema.

57. 59 yo M previous tobacco smoker presented to the ED c/o increased cough, shortness of breath and new sputum production. His CXR on admission was negative for infiltrates or new consolidation (Fig 1.). His baseline PFTs from a year ago are shown above (Fig. 2.). Based on his PFTs and his clinical presentation, what is the most appropriate pharmacotherapy for the treatment of this patient’s condition?
The correct answer is e)
The PFT’s are most consistent with severe COPD. The patient with a moderate COPD exacerbation with increased SOB and sputum production and FEV1 < 50 should be managed with antibiotic therapy in addition to oral steroids and short-acting bronchodilators. Although CHF or PE were not the cause of the patient’s COPD exacerbation, clinicians should consider these diagnoses on the differential since they can often mimic and at times be associated with acute COPD exacerbation, particularly PE in high pre-test probability patients.

58. 64 yo F with history of nasal congestion, conjunctivitis and shortness of breath presented to her PCP for management during the springtime. Previous work up for dyspnea over a year ago showed a CXR with mild bronchial wall thickening and lung hyperinflation. She had a normal TTE and laryngoscopy study in 2014. Biochemical testing showed an IgE level of 742. She had PFTs (shown below) and a methacholine challenge test which caused a drop in FEV1 by 20% at 10 dose units. Based on her clinical history and diagnostic studies, which of the following choices is the most likely diagnosis for the patient’s condition?
The correct answer is d)
Although airflow limitation as demonstrated by reduction in FEV1/FVC < 70% with reversibility with bronchodilator can be seen on PFTs with asthma, the patient’s pattern of hyperinflation and air trapping with an elevated DLCO do support a potential diagnosis of asthma. This pattern in addition to her allergen triggers, elevated IgE level and a positive methacholine challenge test makes allergic asthma the most likely diagnosis. RADS refers to an asthma syndrome which is caused by one large exposure to a noxious agent. Although RADS can have a positive methacholine challenge test, it is not an immune-mediated process. Thus, while the PFTs would look similarly, IgE would not be elevated.

59. 45 yo M presents with increasing dyspnea on exertion over 6 months. He denies cough, fevers, night sweats, or weight changes. He was a previously active non-smoker and has dramatically cut back on his marathon training due to SOB and fatigue. Based on his lung function testing, what disease process is the likely cause for the patient’s clinical presentation?
The correct answer is b)
The patient has a normal FEV1, FVC and FEV1/FVC ratio. His lung volumes are normal. There is no evidence of obstructive or restrictive lung disease. He does have a reduction in DLCO indicating that there is destruction of the alveolar-capillary surface area for gas exchange. Based on his DLCO % predicted he has a moderately reduced diffusion capacity. His isolated DLCO abnormality is suggestive of pulmonary vascular disease.
Based on his spirometry and lung volumes, your next step in his management would be:
The correct answer is d)
Decreased FEV1 and FVC with normal FEV1/FVC ratio and normal lung volumes is a non-specific pattern that can commonly be seen with obesity. Further support of obesity causing the patient’s abnormality is the ERV, which is often decreased on PFTs in obese individuals. The normal DLCO and TLC make a diagnosis of ILD unlikely. A TTE is not indicated at this time due to absence of heart failure history (personal and family) and normal DLCO making PH unlikely. The patient’s PFT pattern is not consistent with obstructive lung disease so adding an ICS is not indicated.

61. Mrs. Taylor is a 42 yo AAF who was referred to your pulmonary clinic for gradually progressive dyspnea. Review of systems is significant for joint aches, myalgias, and photosensitivity with a butterfly rash on her face. She has a PMHx of seasonal allergies and takes occasional OTC antihistamines. Social history is significant for ½ ppd of tobacco smoke for 10 years. She denies any mold in the home, free standing water, or pets. She grew up in Mississippi and recently moved to Atlanta. Her FMHx is positive for a sister with renal failure and some kind of joint disease. An OSH CXR from several years ago indicates that the patient had a pleural effusion. She had PFTs today which are shown.
What part of her history increases her risk for her PFTs abnormalities?
The correct answer is c)
The patient’s PFTs are consistent with restrictive lung disease likely secondary to a connective tissue disease. The patient’s constellation of symptoms seems to best fit a diagnosis of SLE. She would need autoimmune work up to confirm the diagnosis but personal and family history suggestive of SLE supports this diagnosis. The patient has no evidence of airflow limitation due to obstruction, making choice A less likely. Her clinical presentation is not consistent with seasonal allergies, histoplasmosis or age-related decline in PFTs, making B, D and E the incorrect answer choices to this question.

Have feedback about a question or the site as a whole? Please send us an email at pfteach@emory.edu.
